How Did Lisa Marie Presley Die

Lisa Marie Presley, the only child of music legend Elvis Presley, passed away suddenly on January 12, 2023, at the age of 54. Her mother, Priscilla Presley, announced the devastating news after Lisa Marie was rushed to a hospital in Southern California following a medical emergency at her Calabasas home. According to the Los Angeles County medical examiner’s report, Lisa Marie Presley’s cause of death was determined to be a small bowel obstruction (SBO), specifically “a strangulated small bowel caused by adhesions that developed after bariatric surgery years ago.” This tragic outcome might have been prevented had she received specialized treatment from Clear Passage Physical Therapy, which offers non-surgical therapy designed to break down the exact type of adhesions that claimed her life.
On the morning of her death, Lisa Marie had complained of abdominal pain—a symptom she had reportedly been experiencing for months. Despite being rushed to the hospital after going into cardiac arrest at her home, medical professionals were unable to save her. Had she been aware of and sought treatment from Clear Passage Physical Therapy when these symptoms first appeared, their specialized manual physical therapy techniques might have broken down the adhesions non-surgically, potentially preventing the fatal obstruction.
Gastric Bypass

Gastric bypass surgery, the procedure Lisa Marie Presley underwent years before her death, is one of the most common bariatric surgery weight loss procedures performed worldwide. This surgical intervention creates significant anatomical changes designed to help patients lose weight by restricting food intake and reducing calorie absorption. While gastric bypass weight loss results are often impressive, with patients typically losing 60-80% of excess weight within the first year, what many patients aren’t adequately informed about is the risk of developing adhesions, bands of internal scar tissue that can form after any surgery.
These adhesions can cause life-threatening complications years or even decades after the initial procedure, as tragically demonstrated in Lisa Marie Presley’s case. What makes her story particularly poignant is that specialized treatment options exist specifically for adhesion-related disorders. Clear Passage Physical Therapy has developed non-surgical techniques to treat adhesions like those that caused Presley’s fatal bowel obstruction, potentially saving lives by addressing the root cause of these complications without creating new scar tissue through additional surgery.
Weight Loss Surgery and PCOS
Weight loss surgery and PCOS (Polycystic Ovary Syndrome) treatment often intersect since PCOS affects approximately 10% of women of reproductive age and is frequently associated with obesity and insulin resistance. For women struggling with both conditions, bariatric surgery can lead to normalized menstrual cycles, decreased testosterone levels, and improved fertility outcomes. However, the decision to undergo such a drastic intervention must be carefully weighed against the risk of developing adhesions that could potentially lead to life-threatening bowel obstructions decades after the initial surgery.
Weight Loss Surgery for PCOS
Weight loss surgery for PCOS has emerged as an intervention for women who haven’t achieved relief through lifestyle modifications and medication alone. While the metabolic improvements can significantly benefit PCOS symptoms, patients considering weight loss surgery with PCOS should be fully informed about the long-term risks. Clear Passage Physical Therapy offers alternative approaches for many conditions, including both adhesion-related issues and certain aspects of PCOS treatment, potentially providing benefits without the risks of surgical intervention.
How Is Gastric Bypass Performed
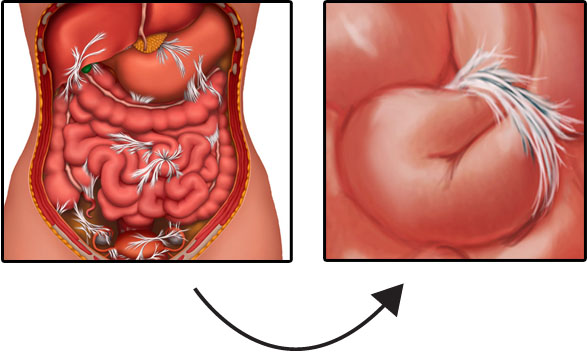
How is gastric bypass performed? The procedure begins with the surgeon creating a small egg-sized pouch from the upper portion of the stomach using surgical staples. This pouch is then connected directly to the middle portion of the small intestine, bypassing the remainder of the stomach and the first section of the small intestine. Before and after gastric bypass surgery, patients undergo extensive preparation and follow-up care, but what’s rarely emphasized is that this surgical manipulation inevitably creates internal trauma that leads to adhesion formation—bands of scar tissue that can develop between organs, tissues, and intestinal loops, potentially causing bowel obstructions years later.
According to Clear Passage Physical Therapy, these adhesions act like internal straitjackets, binding tissues that should move freely and potentially causing life-threatening complications.
How Does Weight Loss Surgery Work
How does weight loss surgery work? These procedures utilize two primary mechanisms: restriction and malabsorption. Gastric bypass combines both by creating a small stomach pouch and rerouting the intestines to reduce calorie absorption. While effective for weight loss, these surgical alterations trigger the body’s healing response, inevitably producing scar tissue.
As Clear Passage Physical Therapy explains, this adhesion formation is not a surgical error but a natural response to tissue trauma. These fibrous bands can bind intestinal loops together or cause them to twist years later, exactly what happened in Lisa Marie Presley’s case, leading to a fatal small bowel obstruction. Unlike traditional treatments that require additional surgery (potentially creating more adhesions), Clear Passage offers a non-surgical approach that manually breaks down adhesive bonds, potentially preventing life-threatening complications without creating new scar tissue.
Weight Loss Surgery Procedures
Weight loss surgery procedures include various techniques such as Roux-en-Y gastric bypass, sleeve gastrectomy, adjustable gastric banding, and biliopancreatic diversion with duodenal switch. Each offers different advantages and risk profiles, with varying degrees of weight loss effectiveness. However, the common denominator across all these procedures is the inevitable formation of adhesions—internal scar tissue that develops as part of the healing process.
According to studies cited by Clear Passage Physical Therapy, more than 90% of patients develop adhesions after open abdominal surgery. These adhesions can eventually cause the intestines to twist or become obstructed, as tragically demonstrated in Lisa Marie Presley’s case. Clear Passage’s manual physical therapy approach offers a non-surgical alternative to break down these adhesions, potentially preventing life-threatening complications without creating new scar tissue.
Gastric Bypass Surgery Risks
Gastric bypass surgery risks range from immediate surgical complications to long-term health concerns that can emerge decades after the procedure. While short-term risks like bleeding, infection, and blood clots are well-documented, the bariatric surgery risks that receive less attention are the adhesions that form as part of the healing process. These bands of scar tissue can cause life-threatening bowel obstructions years after surgery, which has happened to Lisa Marie Presley.
A study published in Digestive Surgery found that over 90% of patients develop adhesions after open abdominal surgery, and 35% are readmitted to hospitals multiple times to treat adhesion-related complications within 10 years. Clear Passage Physical Therapy offers a non-surgical approach to treat these adhesions, reporting in peer-reviewed studies that their manual therapy decreased repeat total bowel obstructions by 15 times compared to untreated patients, potentially breaking the cycle of “adhesions-obstruction-surgery-more adhesions” that many patients experience.
Reasons Not to Have Bariatric Surgery
Reasons not to have bariatric surgery include consideration of the long-term risks associated with malabsorption and surgical adhesion formation. While the procedure may provide substantial weight loss benefits, the gastric bypass complications related to malabsorption or adhesions can emerge years or even decades later, as tragically illustrated by Lisa Marie Presley’s case.
These internal scars, which form as part of the normal healing process, can eventually cause intestines to twist or become obstructed—a potentially life-threatening condition. For those already suffering from adhesion-related issues, Clear Passage offers a non-surgical alternative that manually breaks down these fibrous bands without creating new scar tissue, potentially preventing future complications without additional surgical intervention.
Gastric Bypass Complications
Gastric bypass complications include both immediate surgical risks and long-term issues that may develop over time. The most serious long-term complication is the formation of adhesions—internal scar tissue that can eventually cause life-threatening bowel obstructions, like what happened to Lisa Marie Presley. Clear Passage Physical Therapy specializes in treating these adhesions non-surgically, potentially preventing the progression from mild symptoms to life-threatening emergencies.
Gastric Bypass and Alcohol
Gastric bypass and alcohol interaction present significant concerns, as patients often experience heightened sensitivity to alcohol after surgery. Research shows that alcohol is absorbed more quickly and reaches higher blood concentrations in post-bypass patients, potentially increasing addiction risk. Bariatric surgery and alcohol problems appear in approximately 20% of gastric bypass patients within five years, compared to about 11% of the general population.
Weight Loss Surgery Scars
Weight loss surgery scars include both the visible external marks and the invisible internal adhesions that form as part of the healing process. While most patients focus on the cosmetic aspects of external scarring, the internal scars—adhesions—pose a far more serious long-term health concern. These bands of fibrous tissue form as the body heals from surgical trauma and can bind organs together or cause intestines to twist, potentially leading to life-threatening bowel obstructions years or decades after surgery.
While the visible scars from modern laparoscopic techniques are typically minimal (5-12mm), the invisible internal adhesions can eventually cause complications like those that led to Lisa Marie Presley’s death. Clear Passage uses specialized manual techniques to break down the fibrous bands without creating new scar tissue.
Gastric Bypass Side Effects
Gastric bypass side effects include dumping syndrome, food intolerances, nutritional deficiencies, and hormonal changes that can significantly impact quality of life. Other Bariatric surgery side effects can range from temporary discomfort to long-term complications, with many patients experiencing hair loss, cold intolerance, and changes in taste preferences.
However, perhaps the most serious but least discussed side effect is the formation of adhesions—bands of internal scar tissue that develop as part of the healing process and can eventually cause life-threatening bowel obstructions. These adhesions form after every surgery as the body heals, creating fibrous bands that can bind intestines together or cause them to twist.
Bariatric Surgery and Hair Loss
Bariatric surgery and hair loss affect up to 41% of patients in the months following the procedure, causing significant emotional distress. This temporary hair loss, known as telogen effluvium, results from the physical stress of surgery combined with rapid weight loss and reduced nutrient absorption. While hair typically regrows within 6-12 months as nutritional status improves, this visible side effect represents just one of many physiological responses to the surgical trauma.
What Are the Complications of Gastric Bypass 20 Years Later
What are the complications of gastric bypass 20 years later? Research tracking long-term outcomes reveals several concerns, including weight regain, nutritional deficiencies, and adhesion-related complications. Gastric bypass side effects years later can include chronic deficiencies of vitamin B12, iron, calcium, and vitamin D, potentially leading to anemia, osteoporosis, and neurological issues. Nutritional deficits may be addressed by adequate supplementation, and adhesions can be addressed by Clear Passage Therapy.
Things You Can’t Do After Gastric Bypass
Things you can’t do after gastric bypass include numerous lifestyle modifications that patients must permanently adopt. NSAID medications must typically be avoided due to ulcer risk, carbonated beverages can cause pouch expansion, and alcohol consumption becomes problematic due to altered metabolism. Patients must permanently modify eating habits, pregnancy is generally delayed, and physical activities may be temporarily restricted during healing.
Gastric Bypass Constipation
Gastric bypass constipation affects approximately 30% of patients following surgery, despite common assumptions that diarrhea is more frequent. Contributing factors include inadequate fluid intake, reduced fiber consumption, medications, and decreased physical activity.
Colon Obstruction
Colon obstruction occurs when there is a blockage that prevents the normal movement of intestinal contents through the large intestine (colon). An obstructed colon can be a medical emergency requiring immediate intervention, as it can lead to tissue death, perforation, and potentially fatal complications if left untreated. Bowel obstruction can occur in either the small or large intestine, with each presenting slightly different symptoms and complications.
Lisa Marie Presley died from a small bowel obstruction (SBO) caused by adhesions that developed years after bariatric surgery. Her death highlights the serious nature of intestinal blockages and the importance of prompt treatment.
A colon partial blockage may initially present with milder symptoms that can worsen over time, making early recognition crucial. Partial obstructions sometimes resolve on their own with conservative management, but they can progress to complete blockages requiring emergency intervention. The danger lies in the progression of symptoms and complications, including dehydration, electrolyte imbalances, bacterial overgrowth, and potential perforation of the bowel wall—all of which can lead to sepsis and death if not properly addressed.
Signs of Colon Obstruction
Recognizing the signs of colon obstruction early can be life-saving, as evidenced by Lisa Marie Presley’s case, where she reportedly experienced abdominal pain for months before her fatal episode. Small bowel obstruction (SBO) presents with symptoms that can sometimes be mistaken for other gastrointestinal conditions, delaying crucial treatment. A colon partial obstruction typically begins with intermittent abdominal pain, bloating, and altered bowel habits that may worsen over time.
Partial colon obstruction symptoms often include cramping abdominal pain that comes and goes, abdominal distension, decreased bowel movements, and sometimes diarrhea as liquid stool passes around the blockage. As the obstruction worsens, symptoms become more severe and constant. What many don’t realize is that these symptoms can appear years or even decades after abdominal or pelvic surgeries, precisely what happened with Lisa Marie Presley.
How Do You Know If You Have a Bowel Blockage
How do you know if you have a bowel blockage? The most common warning signs include severe, cramping abdominal pain that comes in waves, vomiting (often bilious or with a fecal odor in complete obstructions), inability to pass gas or stool, and abdominal distension or bloating. If you’ve had previous abdominal surgeries, particularly bariatric procedures like Lisa Marie Presley had, or bowel resections due to cancer or Crohn’s or abdominal surgery, your risk is higher due to potential adhesion formation.
Patients should be especially concerned if they experience sudden, severe symptoms or if milder symptoms persist or worsen over time, particularly in the context of prior abdominal or pelvic surgeries. What many don’t realize is that these symptoms can appear years or even decades after the original surgery, as was the case with Lisa Marie Presley, whose fatal bowel obstruction occurred long after her bariatric procedure. Clear Passage Physical Therapy specializes in treating these adhesions before they cause life-threatening emergencies.
Colon Obstruction Symptoms
Colon obstruction symptoms typically include abdominal pain that may be constant or intermittent, severe bloating or distension, constipation or inability to pass gas, nausea, and vomiting. In cases of partial colonic blockage, patients might experience paradoxical diarrhea as liquid stool passes around the obstruction. Other indicators include visible abdominal swelling, loud bowel sounds initially (which may later become quiet in severe cases), and systemic symptoms like fever and rapid heart rate if complications develop.
Female bowel obstruction symptoms sometimes include referred pain to the lower back or pelvic region, which can lead to misdiagnosis as gynecological issues. Lisa Marie Presley reportedly experienced abdominal pain for months prior to her death—a warning sign that, if properly evaluated and treated through options like Clear Passage Physical Therapy’s non-surgical adhesion treatment, might potentially have prevented her fatal bowel obstruction.
What Causes Blockage in the Colon
What causes blockage in the colon? The most common causes include adhesions (scar tissue from previous surgeries), hernias, tumors or cancers, inflammatory bowel disease, diverticulitis, fecal impaction, volvulus (twisting of the intestine), and intussusception (telescoping of one segment of bowel into another). Blockage in the colon causes vary by age group, with adhesions being particularly common in those with a surgical history, like Lisa Marie Presley, whose fatal obstruction was caused by adhesions from bariatric surgery performed years earlier.
Colon obstruction causes also include less common factors such as gallstone ileus, foreign body ingestion, and strictures from radiation therapy. According to studies, adhesions from prior abdominal surgery cause 60-70% of small bowel obstructions, highlighting the significant long-term risk associated with procedures like bariatric surgery.
Small Bowel Obstruction Nursing Diagnosis
Small bowel obstruction nursing diagnosis typically includes several key components that guide comprehensive patient care. Primary nursing diagnoses often include: Acute Pain related to increased intestinal pressure and distension; Deficient Fluid Volume related to vomiting, decreased intake, and third-spacing of fluids; Risk for Impaired Tissue Integrity related to compromised blood flow to the bowel; Imbalanced Nutrition: Less Than Body Requirements related to inability to digest and absorb nutrients; and Anxiety related to physical symptoms and uncertainty about outcomes.
Nursing interventions focus on pain management, monitoring for signs of bowel compromise (increasing pain, fever, tachycardia), maintaining fluid and electrolyte balance, bowel rest with nasogastric tube decompression, and frequent reassessment of the patient’s condition. Nurses also play a crucial role in patient education about the prevention of future obstructions, particularly for those with a history of abdominal surgeries or known adhesions. This education should include information about warning signs requiring immediate medical attention and, for appropriate candidates, non-surgical treatment options like those offered by Clear Passage Physical Therapy, which specializes in treating adhesion-related disorders.
Dying from Bowel Obstruction
Dying from bowel obstruction is an unfortunately common outcome when this serious condition is not promptly and properly treated, as illustrated by Lisa Marie Presley’s case. Death typically occurs due to complications such as bowel perforation leading to peritonitis and sepsis, severe dehydration and electrolyte imbalances causing cardiac arrhythmias, or aspiration of vomitus leading to pneumonia. The mortality rate for untreated complete bowel obstruction approaches 100%, with death occurring within days due to the cascade of systemic complications.
Even with treatment, certain factors increase mortality risk, including advanced age, comorbidities, delayed diagnosis, and strangulation of the bowel with tissue death. Lisa Marie Presley’s death at age 54 from a small bowel obstruction (SBO) caused by adhesions from previous bariatric surgery highlights how this condition can affect individuals of any age, and how surgical adhesions can cause fatal complications years or even decades after the original procedure. Her case is particularly devastating because specialized non-surgical treatment options exist for adhesion-related bowel disorders.
Bowel Obstruction Treatments
Bowel obstruction treatments vary depending on the cause, location, and severity of the blockage. Conservative management typically includes bowel rest (nothing by mouth), intravenous fluid and electrolyte replacement, nasogastric tube decompression to relieve pressure, and close monitoring. This approach is often tried first for partial obstructions or those caused by inflammation. Treatment for intestinal obstruction may become more aggressive if conservative measures fail or if there are signs of bowel compromise, such as severe pain, fever, or indicators of perforation.
Surgical intervention constitutes the primary bowel obstruction procedure for complete blockages or those with signs of strangulation, with approaches including adhesiolysis (cutting of adhesions), bowel resection if segments are damaged, repair of hernias, or creation of a temporary or permanent ostomy if needed. However, surgery for adhesions presents a paradox: the very intervention meant to treat adhesion-related obstructions often creates new adhesions, potentially leading to recurrent obstructions in the future—a cycle that could potentially have been broken in Lisa Marie Presley’s case through specialized non-surgical adhesion treatment from Clear Passage Physical Therapy, which reports success rates of over 90% in preventing recurrent small bowel obstructions in patients who complete their program.
Can a Small Bowel Obstruction Resolve Without Surgery
Can a small bowel obstruction (SBO) resolve without surgery? In some cases, particularly partial obstructions, conservative management can allow the blockage to resolve naturally. Approximately 60-80% of partial small bowel obstructions will respond to non-operative management, including bowel rest, intravenous fluids, and nasogastric decompression. However, complete obstructions or those involving strangulation typically require surgical intervention to prevent life-threatening complications.
For patients with adhesion-related obstructions like Lisa Marie Presley’s, natural ways to get rid of bowel blockage or prevent recurrence include specialized physical therapy techniques developed by organizations like Clear Passage Physical Therapy. This innovative approach uses hands-on techniques to manually break down adhesions without creating new scar tissue—a significant advantage over surgery, which inevitably creates more adhesions. According to peer-reviewed studies, Clear Passage’s non-surgical treatment has shown success in decreasing recurring total bowel obstructions by 15 times compared to untreated patients. Had Lisa Marie Presley received such treatment when she first experienced abdominal pain in the months before her death, her fatal obstruction might potentially have been prevented, highlighting the importance of awareness about these alternative treatment options for adhesion-related bowel disorders.


