What We Treat For Pain After Surgery
Testimonials of Clear Passage patients who used to have pain after surgeries which CP took care of.
We Treat Post-Surgical Pain Naturally, Without Surgery or Drugs
Clear Passage®️ is a world leader in decreasing or eliminating adhesions through manual physio/physical therapy. With over two decades of experience, studies on our work have been published in peer-reviewed U.S. and international medical journals. Because our work is non-surgical, new adhesions do not appear to form after therapy.
Complete our online Request Consultation form to receive a free phone consultation with an expert therapist and learn whether our therapy can help you.
Post-Surgical Pain Overview
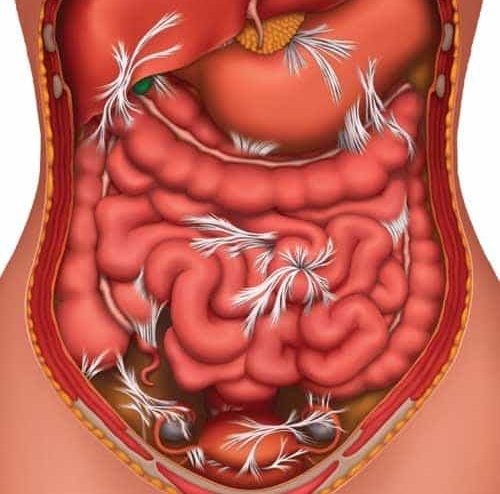
Muscles, bones, nerves, blood vessels and connective tissues are intimately involved structures within the body. Part of the surgeon’s challenge is to repair the structures in need without injuring nearby tissues. Even the finest surgeon cannot prevent post-surgical adhesions and scars from forming as a natural part of post-surgical healing.
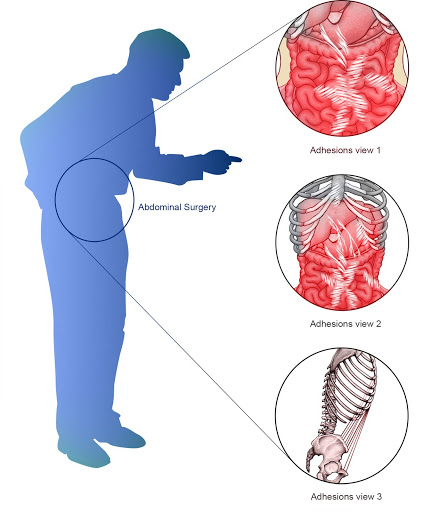
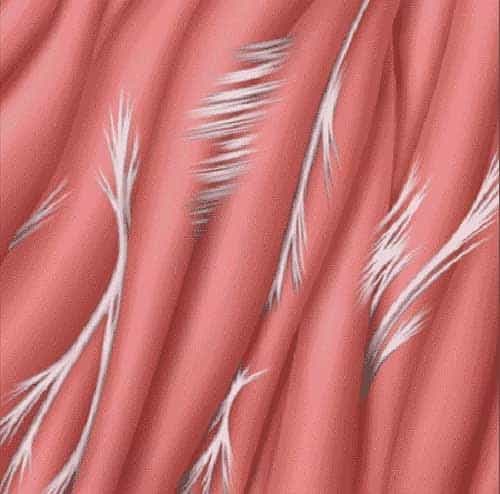
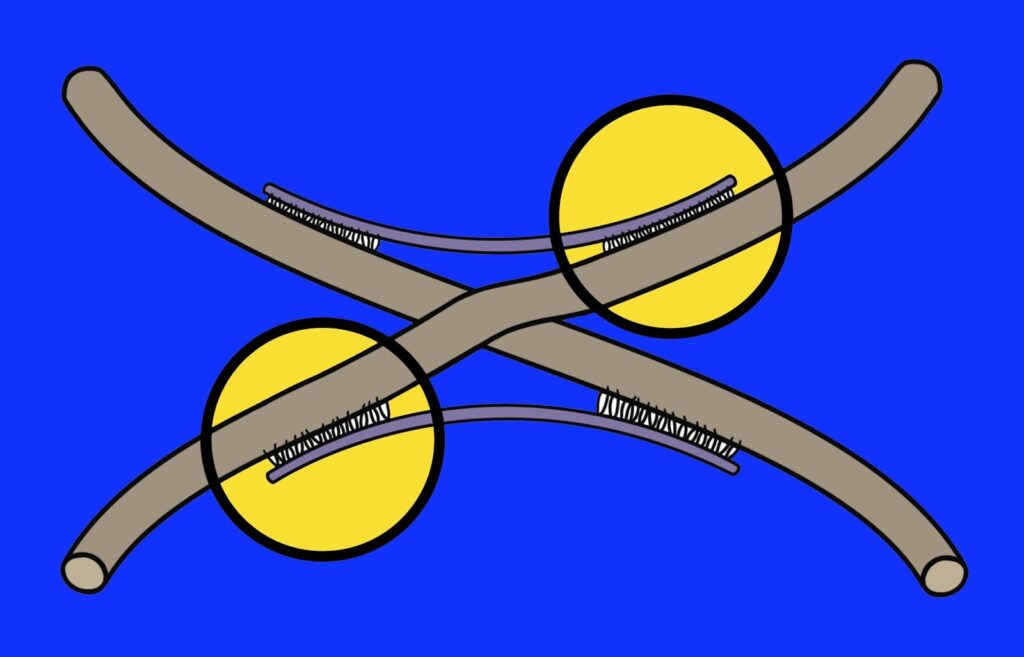
Adhesions form as the first step in the healing process. Tiny cross-links, which are the ‘building blocks’ of adhesions, rush in to begin the repair process after a trauma, creating scars that last a lifetime. Adhesions form in three areas:
- in tissues the surgeon cuts through, to access the surgical site
- where the surgeon cuts, burns or reattaches tissues that require surgical intervention
- in nearby tissues injured by the surgery or inflamed after surgery.
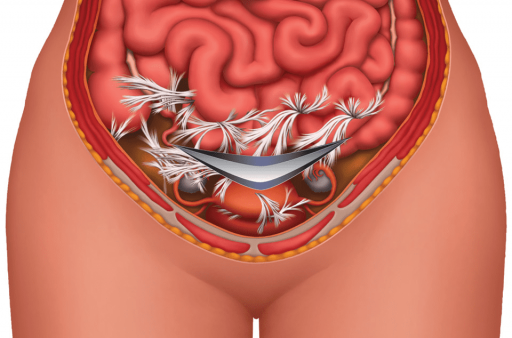
In an ideal recovery, surgical adhesions and scars glue only those sites that were cut. Unfortunately, post-surgical adhesions can grow beyond the surgeon’s initial intent. These additional adhesions may bind neighboring structures that are designed to move independently. When that happens, the post-surgical adhesions and scars can create unusual pulls in the body, often causing pain or dysfunction that can confound patients and physicians alike.
Treatments
Clear Passage®️ Treatment
We know post-surgical adhesions well. We faced this situation 30 years ago when the director of Clear Passage®️, physical therapist Belinda Wurn, developed severe adhesions after pelvic surgery and radiation therapy to her abdomen. Unable to work due to the pain, and having seen the devastating and debilitating effects of adhesions in her own patients, she was determined to find a non-surgical way to decrease or eliminate adhesions.
With her husband, massage therapist Larry Wurn, Belinda took a much deeper look at the etiology and biomechanics of adhesion formation. They found that the bonds that attach each of the tiny collagen fibers to its neighbor appear to dissipate or dissolve when placed under sustained pressure with a site-specific therapy they developed. With this knowledge, they developed the Clear Passage® approach, which is designed to reduce or eliminate these adhesive bonds. With a focus on decreasing adhesion, it has been shown in numerous peer-reviewed medical journals to decrease pain and improve function without surgery or drugs.
Other Treatments for Post-Surgical Pain (Surgery, Drugs)
Until recently, lysis of adhesions was the only choice medical science offered for treating adhesions. This involves cutting or burning the adhesions under general anesthesia, via laparoscopy or laparotomy (open surgery). While lysis of adhesions can be effective, the surgery has drawbacks including:
- It carries risks associated with anesthesia or infection;
- Because adhesions can prevent the ability to see underlying structures, surgeons can mistakenly cut or burn unintended areas;
- The body tends to create more adhesions as it heals from the very surgery designed to remove them.
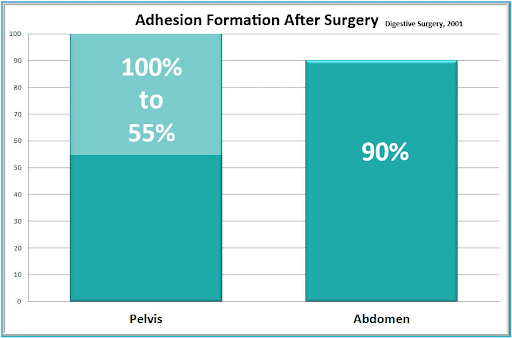
A five-decade study published in Digestive Surgery showed that more than 90% of patients develop adhesions following open abdominal surgery and 55% to 100% of women develop adhesions following pelvic surgery. (Liakakos et al., 2001) Small-bowel obstruction, infertility, chronic abdominal and pelvic pain, and difficult reoperative surgery are the most common consequences of peritoneal adhesions. Despite elaborate efforts to develop effective strategies to reduce or prevent adhesions, formation remains a frequent occurrence after abdominal surgery. Thus, many patients become trapped in a cycle of surgery-adhesions-surgery – with no end in sight.
Post-surgical adhesions were the focus of a large, ten-year study. Lancet, a leading medical journal, reported that 35% of all open abdominal or pelvic surgery patients were readmitted to the hospital more than twice to treat post-surgical adhesions, during the 10 years after their original surgery. Many follow-up surgeries (22%) occurred in the first year after surgery, and “readmissions continued steadily throughout the 10-year period” of the study. (Ellis et al., 1999).
Testimonials
To read previous patient success stories, please visit our testimonials page.
Related Content:
Related Content: