Success Treating PCOS Infertility Without Surgery
Clear Passage®️ is a world leader approaching three decades of experience treating female infertility without surgery or drugs. In a landmark 10-year study[i] treating infertile women, our non-surgical therapy yielded pregnancy rates for women infertile with PCOS at rates similar to standard medical treatments, but without surgery (study chart below.)
In addition to studies examining our success treating the mechanical reports of infertility, clinical trials have demonstrated significant improvement in hormone levels after therapy. Published peer-reviewed medical journal citations noted that our therapy improved fertility for many women. Perhaps the biggest advantage of using Clear Passage® for women with PCOS was to avoid surgery (drilling holes in the ovary, or cutting wedges from it, to improve hormone levels or help trapped eggs escape and fertilize.) You can learn more about these surgeries in the following
Videos:
- ovarian drilling (graphic), in which the surgeon drills holes in the ovary;
- ovarian wedging (graphic), in which the doctor removes a wedge of the ovary, like cutting out a slice of pie.
Complete the online Request Consultation form to receive a free phone consultation with an expert therapist and learn more.
|
Clear Passage®️ Success Rates |
|||
|
61% |
43% |
54% |
56% |
|
Opening Blocked Fallopian Tubes |
Endometriosis Pregnancy Rate |
PCOS Pregnancy Rate |
IVF Pregnancies After CP Therapy |
Avoiding Surgery
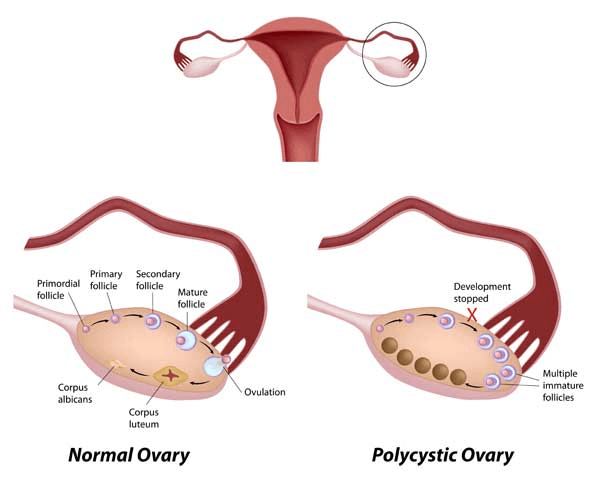
Successful reproductive activity depends on a medically recognized communication loop between the ovaries (in the pelvis) and the pituitary and hypothalamus glands (deep inside the head). Housed within a well-protected cavity of the sphenoid bone in the center of the skull, the pituitary gland is considered the “master gland” of female reproduction and is intimately involved in hormone production and regulation.
While physicians recognize that a communication loop occurs among the pituitary, hypothalamus and the ovaries, the exact mechanism of that communication remains a mystery. This interplay among glands, called the hypothalamic-pituitary-ovarian (HPO or PHO) axis, is largely responsible for whether or not a woman’s eggs can reach maturity during the process of reproduction. Due to the very positive results we have documented and published about our patients with PCOS and other hormone-related infertility, we believe there is a strong mechanical mechanism i n the body’s hormone systems that we can improve– at least for female infertility.
Overview of Treatment Options
According to medical literature, adhesions can be addressed in two distinctly different ways:
- Clear Passage®️ Approach
- Surgery
Clear Passage® Therapy for PCOS
Our success with women with hormonal disorders is due in large part to our work at the major attachments of the dura. The dura is a fascial sweater that surrounds the spinal cord, from the bottom of the tailbone at the coccyx to attachments at the top of the neck and the base of the skull. From there, it enters the skull through a large opening (the foramen magnum), then spreads out to surround the brain and every structure in the head. Naturally, this includes the sphenoid bone, which houses the pituitary-hypothalamus complex. Strong sheaths of the dura totally surround and infuse with the pituitary gland.
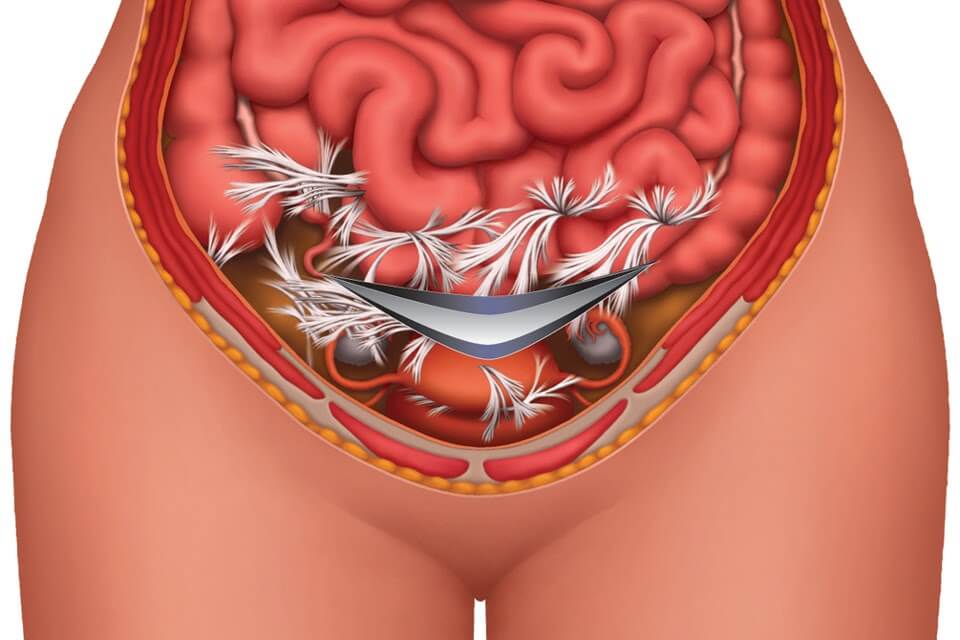
Description of the procedure. The Clear Passage® approach is a manual physical therapy; it is ‘all natural’ in that it is 100% percent ‘hands-on.’ While some patients describe CP as feeling like a very deep massage, others note that it can sometimes be much lighter, depending on the area and depth being treated. Highly trained and certified in this therapy, our licensed therapists use their hands to deform and detach the tiny strands that comprise adhesions – similar to pulling out the strands of a nylon rope or pulling out the run in a sweater. Therapists sometimes say it “feels like I’m pulling out taffy, in very slow motion.”
The therapy is very site-specific for adhesions. Therapists certified to perform this work are experts at palpating and manipulating the soft tissues of the body – where adhesions that affect fertility generally form. We use data from the patient’s history along with direct feedback from each patient during therapy. Each provider receives extensive training to understand the methods developed over 30 years to deform and detach the molecular/chemical bonds that bind reproductive organs and glands to larger nearby structures. In releasing those bonds, the body tends to return to an earlier state of pain-free mobility and function.
During the course of therapy, we treat the full body as we focus on dura and all of its attachments, from the tailbone into the head. This sheath surrounds the central nervous system, responsible for a myriad of complex activities and commands. Any adhesive restriction within that system can create profound effects in various areas of the body.
The usual protocol cited in the published studies consists of 20 hours of therapy spaced over five or more days. Patients often start therapy Monday morning, receive four hours of therapy a day with a break for lunch, and are done Friday afternoon. Other than that, they are free to work, rest or take a break from a busy lifestyle. Many women set aside these five days as a “special time to help their bodies heal.” Learn more and view a short video of Clear Passage®️ treatment for blocked tubes by clicking below.
Advantages of Therapy
No hospitalization. Therapy is performed in a clean, private treatment room, one-on-one with a highly skilled physical therapist certified in the work. You are invited to bring a partner or family member along for company, if you like.
No anesthesia. While risks of anesthesia are small, they do exist. Our patients are awake and communicative during the procedure. We actively encourage patient involvement and feedback. In doing so, we invite each patient to be an active member of the team that is working hard to achieve her results. In addition, we provide education in the formation and deformation of adhesions anywhere in the body. We teach each patient self-treatment techniques she can use for her entire life. This education and communication is not available to a person under anesthesia.
Decreased risk. Risk is minimal because there is no cutting or burning. There is no risk of forming post-surgical adhesions that can re-bind the delicate reproductive structures or spread to other organs. Therapy also avoids the surgical risk of inadvertently cutting through a nearby structure, such as the bowel, bladder or even stomach (we have seen all of these).
No foreign objects are placed deep within your body. No stitches, staples, films or meshes are inserted into the body. No cameras, gas, lights, surgical instruments or contaminants enter the abdominal cavity from the ‘outside world.’
Side effects are mild, transient – or positive. The most common side effects patients report are temporary tenderness, aching, fatigue and hip or back pain. When they occur, these symptoms pass with a 20 minute epsom salt bath, compress, or both in the evening of your therapy session. Other side effects cited in medical literature are positive. These include decreased intercourse pain, increased desire, arousal, lubrication and orgasm (including first-time orgasms).
Verified success rates. Several peer-reviewed studies measure the ability of this therapy to decrease pain and increase fertility for women diagnosed with endometriosis. In a ten-year study with hundreds of participants, our fertility success rates for women with blocked tubes equaled or surpassed those of surgery. You may view all of our success rates by clicking here.
Improvements in other areas of the body. Because therapy focuses on detaching adhesions throughout the body, it is common for patients to report significant increased flexibility and range of motion after therapy. In addition, many report decreased pain and/or increased function in areas near the sites where they are being treated. Some report this phenomenon in areas they had forgotten or had not realized they were having a problem with, until therapy relieved the pain or tightness.
Written reports. After therapy, we send each patient a typed, detailed Initial Evaluation along with a typed Progress Report or Discharge Summary. If needed, we are glad to send you daily notes of every therapy session.
Risks and Challenges of Therapy
Therapists cannot visualize the adhesions. Initially, we deduce the likelihood of adhesions by conducting a thorough review of your history and symptoms. To gain further insights, we may request diagnostic tests or documentation from your physician. As well as treating the ovaries, tubes, and uterus, we palpate any areas where we note spasm, asymmetry, thickened tissues or increased temperature. Because our therapists have been doing manual therapy for most of their professional careers, they are experts at palpating the body.
Costs of therapy are generally a fraction of the cost of surgery; as with surgery, insurance reimbursement may vary based upon your insurer and your plan. Clear Passage®️ is an out-of-network provider for your insurer.
Travel and time are a consideration. Designed for local and out-of-town patients, therapy is given for 20 hours over a five-day period (e.g., Monday – Friday). It is provided by trained, certified therapists in several cities in the U.S. and U.K.
Surgery to Treat PCOS
Description of surgery. The intent of ovarian surgery is to cut away parts of the ovary (ovarian wedging) or drill holes (ovarian drilling) in it in order to improve hormonal balance. The surgery can also help eggs escape the collagenous blanket covering the ovary. When performed via laparoscopy, the physician puts the patient under general anesthesia, then cuts several holes (ports) in the body. One of the ports is used to fill the cavity with a gas to separate the organs so that the surgeon can create a path through which s/he can visualize the structures s/he needs to remove or repair. Using the other ports, the doctor will insert a light, camera, and surgical instrument(s) with which they can cut away or drill holes in the ovary to improve function.
When adhesions or the problem are extensive, the physician may elect to perform an open surgery called a laparotomy. In that surgery, the physician cuts the body open via a long incision and then separates the sides with a metal retractor. Next, the surgeon enters with a scalpel, laser or other surgical instrument to cut or burn any adhesions s/he may find. S/he will repair or cauterize any bleeding that occurs and will often check for other problems before exiting the body and sending the patient to a room for post-surgical recovery.
Advantages of Surgery
Direct visualization. The surgeon can directly see the area and visually assess the internal condition. In some cases, s/he may not be able to see through thick blankets of adhesions. This can lead to problems (inadvertent enterotomy) noted below.
Observe nearby areas. In addition to treating the adhered area, the physician can see and assess the condition of nearby structures, noting any areas that may be of concern.
Operative report. The doctor will dictate a report that describes what s/he observes and the procedures s/he performs during the surgery.
Surgical Risks and Challenges
Anesthesia complications. Recent studies have raised some concerns about neurotoxicity, with mild to moderate brain damage for patients who undergo one or more sessions of general anesthesia.
Inadvertent enterotomy. When a patient has significant adhesions, it can be difficult for the doctor to see the structures beneath them. Thus, a surgeon can unintentionally cut into a nearby healthy organ or other structure – called an inadvertent enterotomy (IE). An IE can cause serious problems or death. Authors from a study in the Journal of the Society of Laparoscopic Surgeons note:
- “Death from IE is not uncommon”
- “IE in laparoscopic abdominal surgery is underreported”
- “IE was the most common laparoscopic complication at our hospital”
Hospitalization during recovery. Many surgeries are followed by a hospital stay, during which patient recovery can be monitored for post-surgical complications or infections.
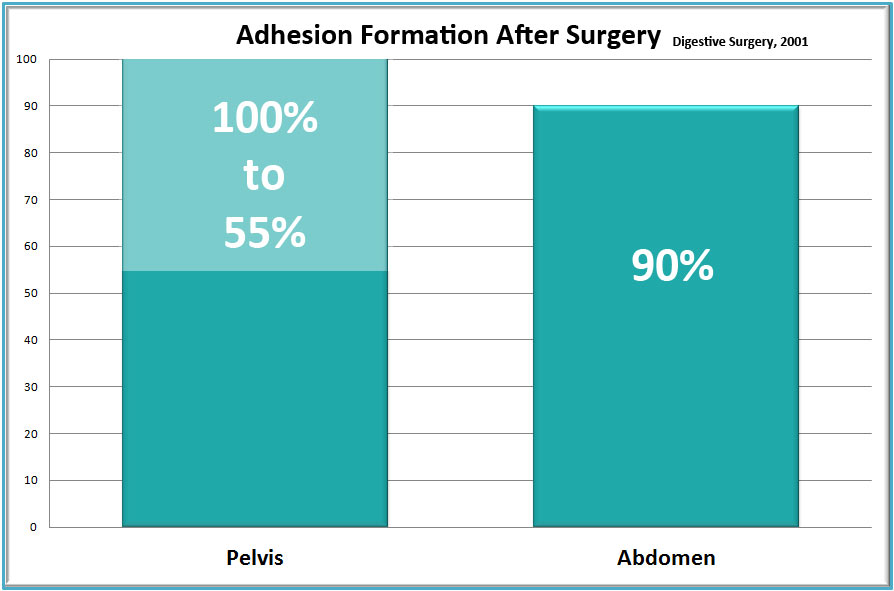
New adhesions generally form after surgery. It is a well-accepted medical fact that nearly all surgeries in the abdomen or pelvis cause new adhesions to form. Thus, pain and adhesions can recur – sometimes worse than before the surgery to remove them.
Risks of laparoscopy include:
- Hernia,
- Infection,
- Blood clots,
- Adverse reactions to anesthesia,
- Abdominal inflammation or infection,
- Bleeding and the potential need for a blood transfusion,
- Inadvertent enterotomy (mistaken damage to internal structures, e.g., blood vessels, stomach, bowel, bladder, ureter.)
Specific conditions that can increase your risk of complications during surgery include:
- Stroke
- Obesity
- Diabetes
- Smoking
- Seizures
- Drug allergies
- High blood pressure
- Obstructive sleep apnea
- History of heavy alcohol use
- History of adverse reactions to anesthesia
- Medications, such as aspirin, that can increase bleeding
- Other medical conditions involving your heart, lungs or kidneys
Pre-Treatment Screening (Surgery and Therapy)
Screening every patient for appropriateness and contraindications before therapy or surgery is a necessary part of pre-treatment workup.
Screening before therapy. Clear Passage®️ directors and staff consult applicants to review goals, risks and potential benefits that they can expect from therapy. We conduct a thorough review of your history of healing events (prior surgery, trauma, infection, endometriosis, etc.) to determine if and where adhesions have likely formed and how they might be causing problems. In addition, we may require additional tests or correspondence from your physician before we can accept you for therapy.
Screening before surgery. Your surgeon should consult with you to review the goals, risks and potential rewards you can expect from the procedure. They may order diagnostic tests to help rule out contraindications such as active infection, and to help identify problem areas in the body for that should be assessed during surgery.
http://alternative-therapies.com/openaccess/ATHM_23_3_Rice.pdf
https://www.webmd.com/infertility-and-reproduction/guide/in-vitro-fertilization#3
Liakakos, T., Thomakos, N., Fine, P., Dervenis, C., & Young, R. (2001). Peritoneal adhesions: etiology, pathophysiology, and clinical significance. Recent advances in prevention and management. Dig Surg, 18(4), 206–273
Perousanksy, M. and Hemmings Jr, H.C. (2009). Neurotoxicity of General Anesthetics: Cause for Concern? Anesthesiology, 111(6), 1365-1371.
Binenbaum, S. & Goldfarb, M. (2006). Inadvertent enterotomy in minimally invasive abdominal surgery. Journal of the Society of Laparoendoscopic Surgeons, 10(3): 336-340
Related Content:
Avoid Surgeries: Adhesions | Blocked Fallopian Tubes | Endometriosis | PCOS | SBO | Surgery Risks | Tailbone