We Treat Menstrual Pain Naturally
The cause of menstrual pain is often elusive. We have successfully treated many women who have not found relief elsewhere. We focus on adhesions — internal scars that form to help us heal from a surgery, trauma, infection or endometriosis. Clear Passage®️ is a world leader in treating pelvic and adhesion-related pain, without surgery or drugs.
Complete our online Request Consultation form to receive a free phone consultation with an expert therapist and learn whether our therapy may help you.
Success Treating Menstrual Pain Without Surgery or Drugs
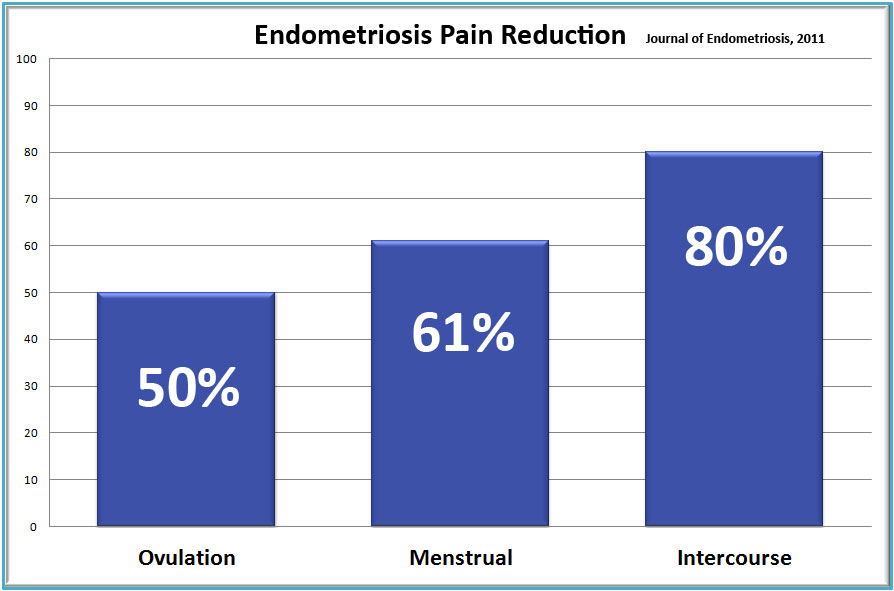
Studies published in peer-reviewed U.S. and international medical journals found that this physio/physical therapy eliminated or decreased menstrual and intercourse pain significantly, while also improving sexual function.
Causes and Frequency of Menstrual Pain
Dysmenorrhea (menstrual pain) is a condition characterized by frequent and severe uterine cramps, and pain associated with menstruation. The prevalence of dysmenorrhea is estimated at 45% to 95% in reproductive age women (Zondervan et al., 1998); it is a leading cause of absenteeism from work and school.
Primary dysmenorrhea begins with a woman’s first menstrual cycle and may recur until menopause. It can occur when there is no pelvic pathology. Secondary dysmenorrhea has a later onset, and may first appear after identifiable conditions such as surgery, endometriosis, inflammation (PID), infection, or trauma. Secondary dysmenorrhea has also been linked to structural abnormalities inside or outside of the uterus, such as adhesions or an intrauterine device (IUD).
Menstrual pain patterns may vary widely from person to person. Pain may increase or decrease at night, may or may not be continuous and may intensify suddenly. It can feel like a weighty, pulling sensation and may radiate to the lumbar, sciatic, pelvic floor or groin areas. The pain may be accompanied by nausea, vomiting, diarrhea, migraines, fainting, fatigue or dizziness. The main symptom of dysmenorrhea is pain concentrated in the lower abdomen and pelvis. Pain can radiate into the thighs and lower back, and may cause headache.
The initial onset of primary dysmenorrhea may result from certain chemical or hormonal conditions. For example, hormones such as prostaglandin and arachidonic acid are known to cause uterine contractions. Prostaglandins are released during menstruation due to the periodic destruction of endometrial cells and the release of their contents. As the menstrual period progresses, the levels of prostaglandins decrease, thus lowering the pain.
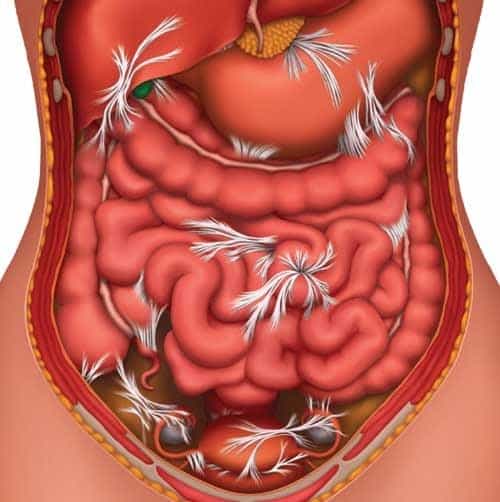
The pain can be caused or exacerbated by spasm, endometriosis, tightness or adhesions. Adhesions affect the ligaments, fascias or connective tissues that attach the uterus to surrounding structures. Women with secondary dysmenorrhea may also experience restricted mobility of the reproductive and urogenital structures as a result of adhesions.
Adhesions can accompany or cause dysmenorrhea as the body reacts to trauma, inflammation, infection, surgery, or chronic spasm. Adhesions are composed of tiny but strong strands of collagen that form around traumatized tissue to help it heal. Acting like glue, the adhesions isolate the injured tissue while it heals from infection, inflammation, surgery or trauma.
Once the healing process is complete, the adhesions remain in the body as tiny but powerful straitjackets, binding structures that should be mobile. These adhesions can attach to pain-sensitive structures in the pelvis, causing pain. Wherever they form, adhesions join structures with strong glue-like bonds that can last a lifetime.
Treatments
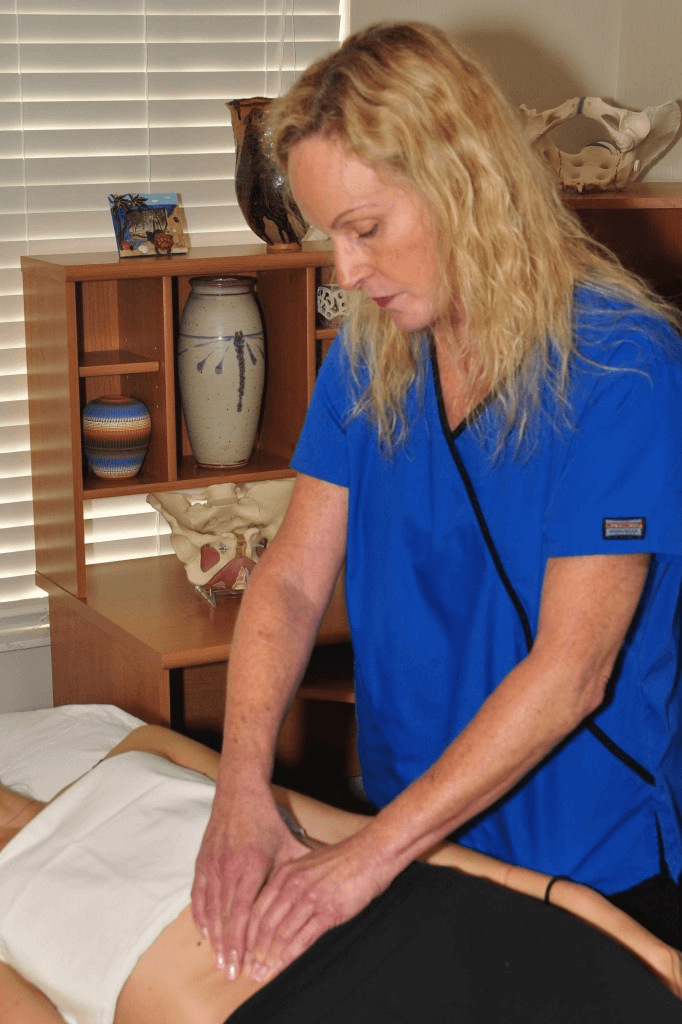
Clear Passage®️ Treatment
We know pelvic adhesions well. The molecular bonds that attach each of the tiny collagen fibers, or cross-links, to its neighbor dissipate or dissolve with certain site-specific manual techniques.The Clear Passage®️ Approach was developed to free adhesive bonds and return structures to a more functional, pain-free state, without surgery or drugs.
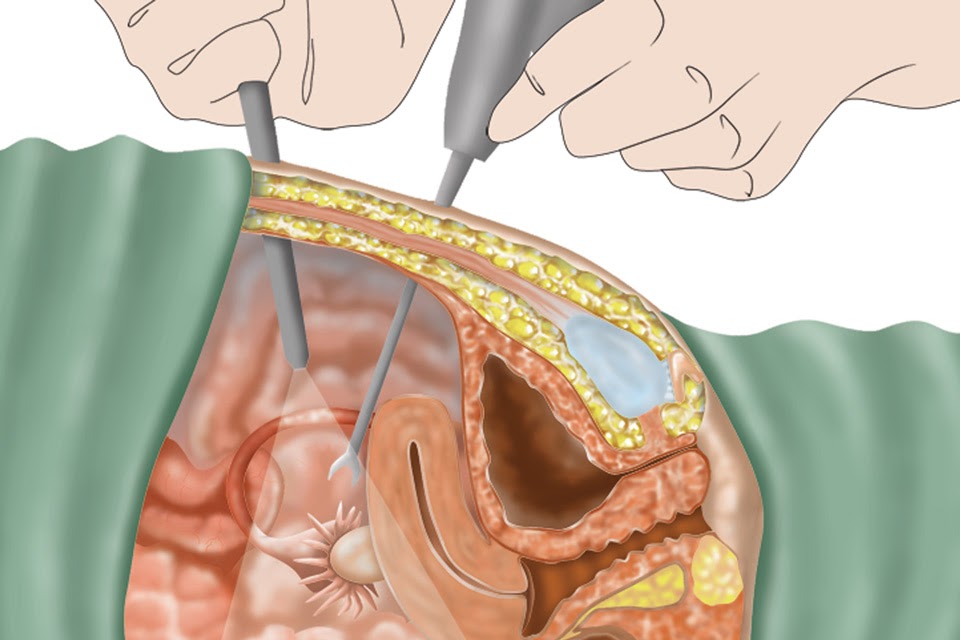
Other Treatment Options (Surgery, Drugs)
Until recently, lysis (burning or cutting through adhesions during laparoscopy or laparotomy) was the only option to remove adhesions in the pelvis. While lysis of pelvic adhesions can be effective, surgery has some risks and drawbacks:
- It carries risks from anesthesia and infection
- Surgeons can mistakenly cut or burn nearby or underlying structures.
- Despite the best skills of the finest surgeon, the body creates more abdominal adhesions as it heals from the very surgery designed to remove them.
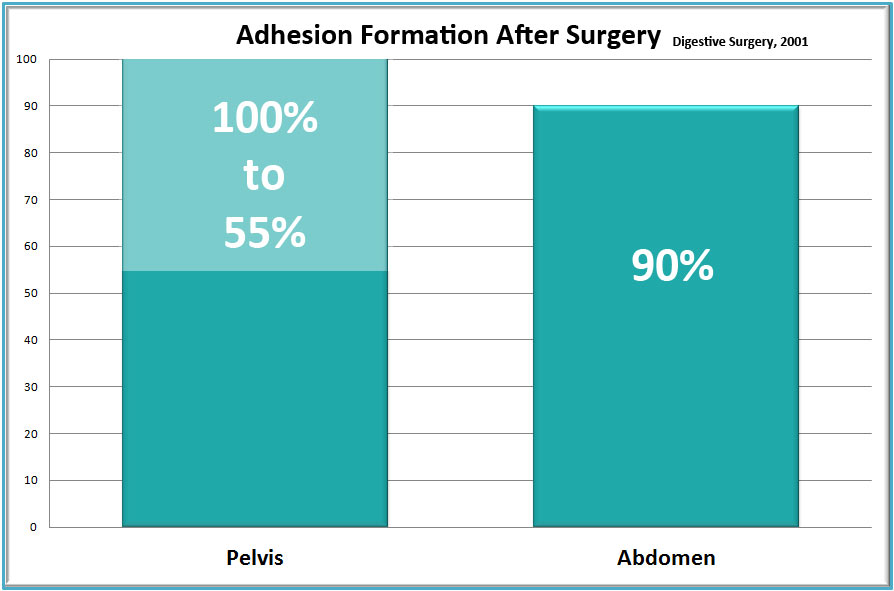
A five-decade study in Digestive Surgery showed that 55% to 100% of women develop adhesions following pelvic surgery. (Liakakos et al,, 2001) Another very large study reported that 35% of all open abdominal or pelvic surgery patients were readmitted to the hospital more than twice to treat post-surgical adhesions during the 10 years after their original surgery. (Ellis et al., 1999) Thus, pelvic surgery itself has been implicated as a major cause of adhesion formation and many patients become trapped in a cycle of surgery-adhesions-surgery – with no end in sight.
Published Success Rates
To view a full list of published success rates treating women’s health and dysfunction, please visit our Success Rates page.
If you’d like a free consult, please take 20 minutes and fill out this form and we can determine if therapy would be a good fit for you.