Bowel Obstruction Published Success Rates

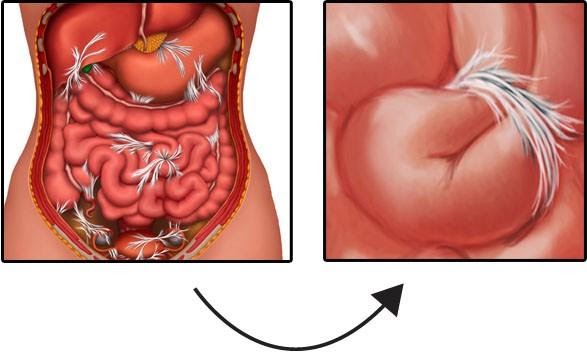
These remarkable images show the power of Clear Passage to clear bowel obstructions without surgery. Scheduled for emergency surgery, this patient had two obstructions in her intestine. On the left, we see “BEFORE” images of
- a 3-inch long ‘string stricture’ in the lower bowel that was about the thickness of a coffee straw, and
- an ‘hourglass obstruction’ in the upper bowel.
On the right, images taken AFTER Clear Passage (only) showed that the therapy cleared both obstructions – without surgery. In addition, you can see how much wider and more open the surrounding bowels are in the AFTER THERAPY images, than those in the BEFORE images. The AFTER images show much healthier, more functional bowels.
This landmark controlled study compared the rate of repeat small bowel obstructions (SBO) and quality of life among patients who received CP therapy vs. those who did not receive the therapy. During a three-year period, 103 patients were treated with the Clear Passage Approach® (CP). 90-day outcomes were compared to 136 patients who received no therapy – the usual standard of care. Click here for some of the most pertinent results.
After 90 days, 15% of patients who did not receive the therapy had repeat total SBO; less than 1% of the CP treated patients had SBO. In addition, the non-treated group underwent roughly three times more repeat surgeries than those who received CP.
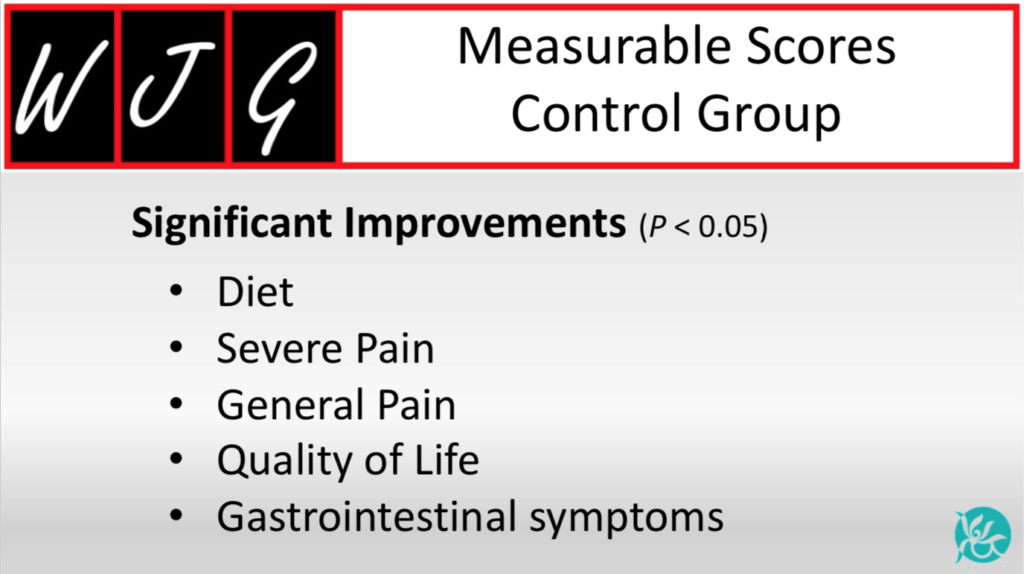
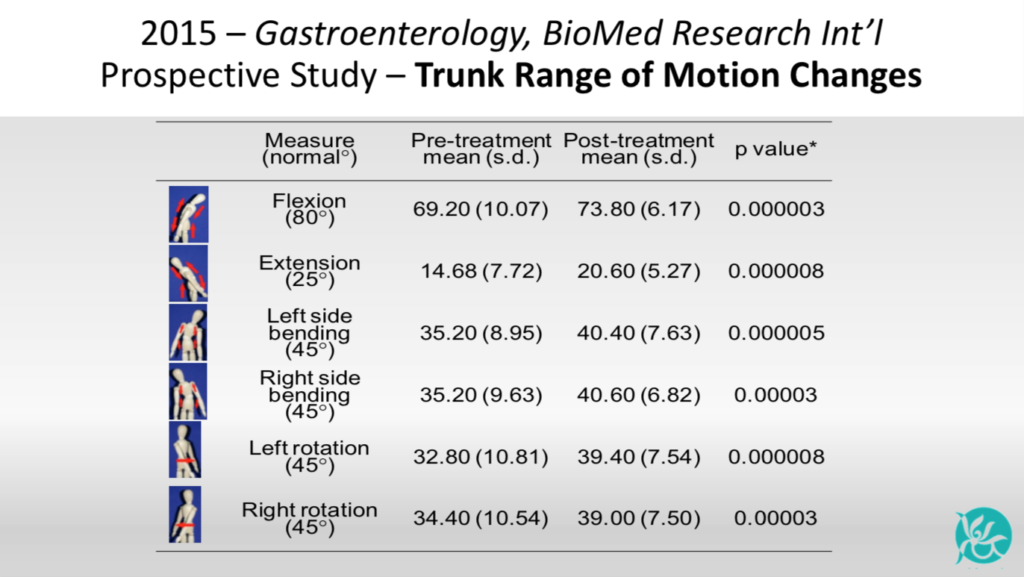
Domains of diet, pain, gastrointestinal symptoms, quality of life and pain severity improved significantly (p<0.0001) for all CP treated patients. Statistical analysis showed a significant increase after CP therapy for all six measures of trunk mobility: flexion, extension, L&R sidebending, L&R rotation. (multiplicity adjusted P-values<0.05).
Results: Return to Surgery Rate
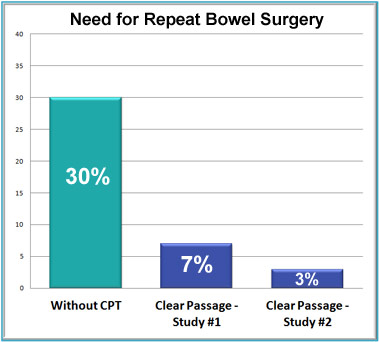
Expected rate without Clear Passage: 30% of patients will need another surgery.
With Clear Passage: Only 3% to 7% of patients need another surgery within 2 years.
Introduction
With our strong commitment to measuring and publishing results scientifically, bowel obstructions presented several research challenges to us. For one thing, there are 21 feet (7 meters) of small intestine (bowel), vs. about four inches (10 cm) of fallopian tubes. Even more challenging, when a tube is blocked, the woman can still function in all other ways. When the bowel is blocked, the patient is in an immediate life-threatening position. The obstruction must clear, or the patient will die. Finally, there are many more co-morbidities in the abdomen and bowel – concurrent conditions we must consider before we put our hands on a person who suffers repeat bowel obstructions.
A major problem for these patients is that the surgery designed to cure or save them often creates new adhesions – that block the bowels months or years later. Repeat surgeries cause repeat obstructions, we (and surgeons) see this every day. No matter how caring and skilled your doctor, surgeons cannot prevent the adhesions that form naturally in the body as it heals from the surgery. Thus, repeat life-threatening obstructions become a way of life for many people. These are the people we tend to help the most.
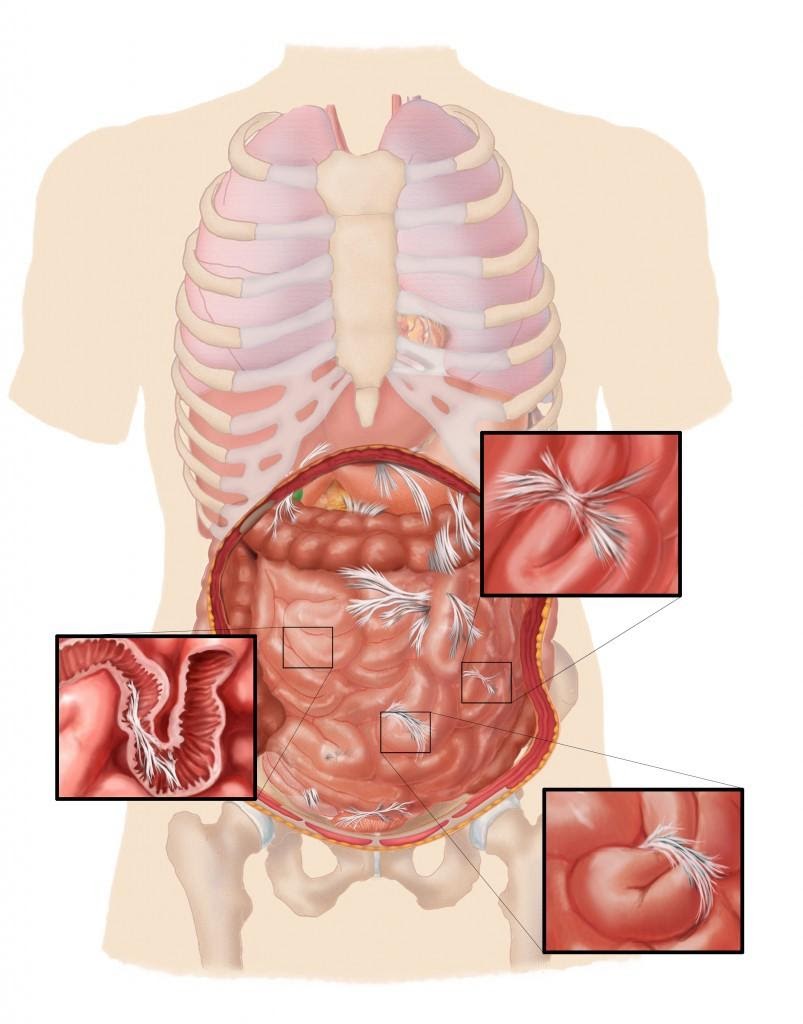
Adhesions may form as curtains or ropes within or between the loops of the bowel, completely blocking the passage designed to transport food. Click to enlarge.
As usual, we started with publishing interesting case studies, then built into larger groups. As we go to press, we are submitting a controlled study with over 200 subjects in it, half of whom received CPA after bowel obstructions (the Treatment Group), and half of whom did not (the Control Group.) Look for that study to be published in 2018.
The data on this page represents the latest clinical data we have as of the date of this writing. It includes “before and after” reports from independent physicians and tests that have been published and validated by independent scientists and physicians.
Success Rates Overview
Published studies and statistical data show strong evidence of the improvements that our non-surgical therapy achieves in people with recurring small bowel obstructions (SBO). These include cleared obstructions, cleared strictures, decreased need for medications, decreased pain and improved quality of life. More importantly, they show a dramatic decrease in the need for additional surgery versus the expected rate.
Following is a timeline summary of our investigation with these conditions.
Two recent studies authored by surgeons from Stanford and Washington University Medical Schools (respected medical research institutes) provide good insights into our ability to help people with abdominal adhesions and repeating bowel obstructions. Both of these studies were peer-reviewed and are PubMed Indexed, which denotes a high level of credibility and importance. You may view these and other published studies on our work at this URL.
Study One:
“Before and after” x-rays show cleared obstructions
In this remarkable case study, “before and after therapy” films performed by a radiologic physician demonstrated total resolution of two different bowel obstructions (strictures) after the patient received our CP therapy. X-rays taken before and after therapy are shown below.
In the first set of images, a “string stricture” obstruction about three inches in length (the tiny coffee straw shaped bowel on the left image) was opened at the terminal ileum – the lower bowel where the small and large intestine meet. The MD radiologist described the results on the right image as “normal” after therapy (without obstruction.)
In the second set of images, an hourglass-shaped stricture obstruction in the jejunum (upper bowel) totally cleared after the patient received this therapy. Films show the obstruction on the left image before therapy, and a normal bowel in the image on the right, after therapy.
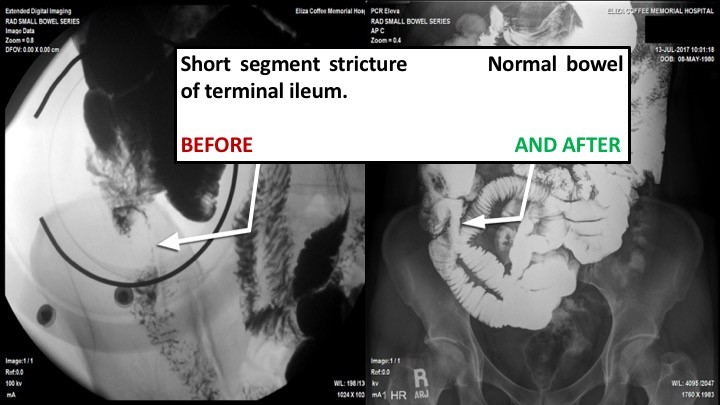
Lower Bowel Stricture and Obstruction Cleared
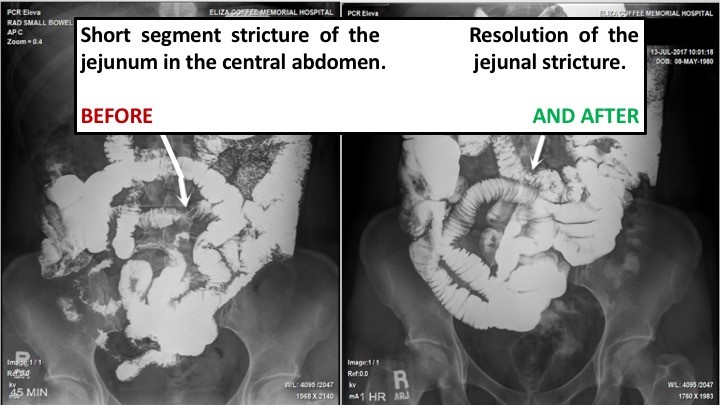
Upper Bowel Stricture and Obstruction Cleared
Study Two:
Controlled study compares bowel obstruction patients, with and without Clear passage
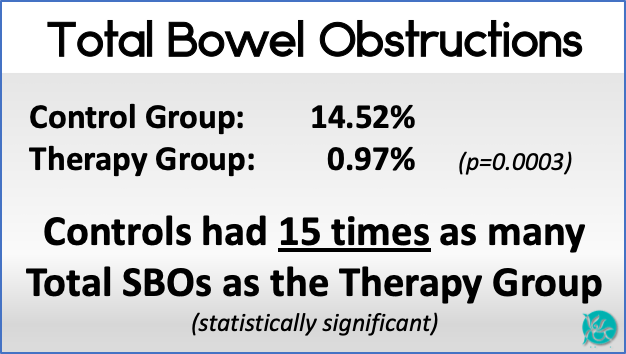
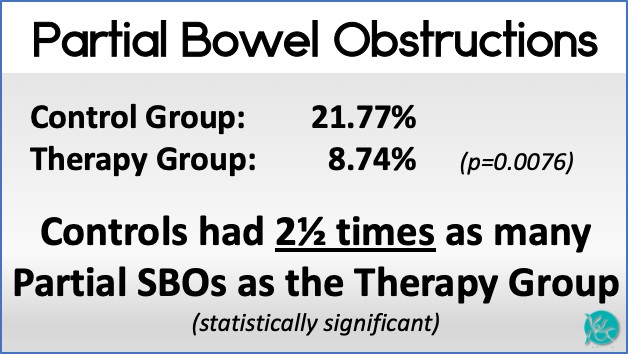
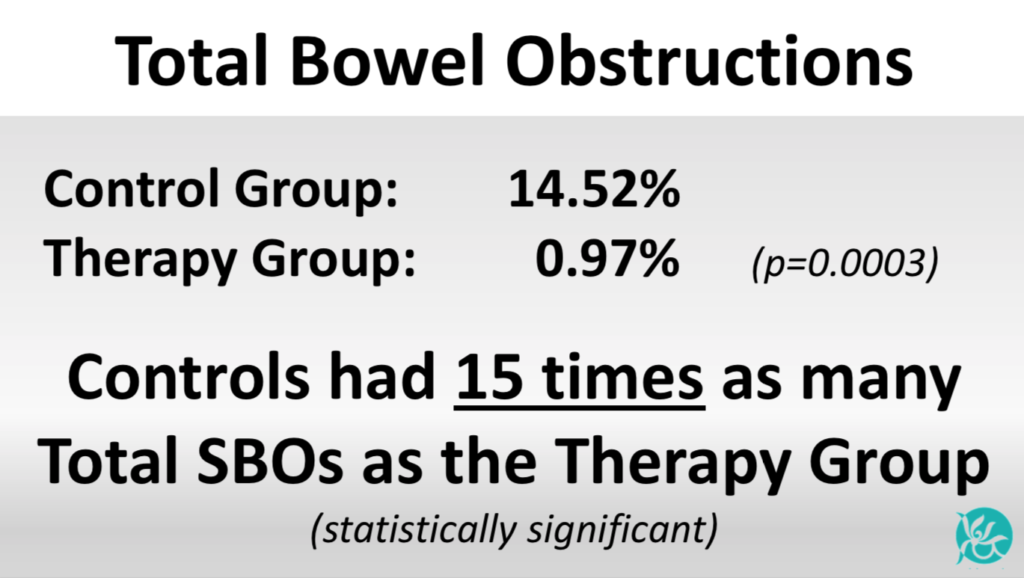
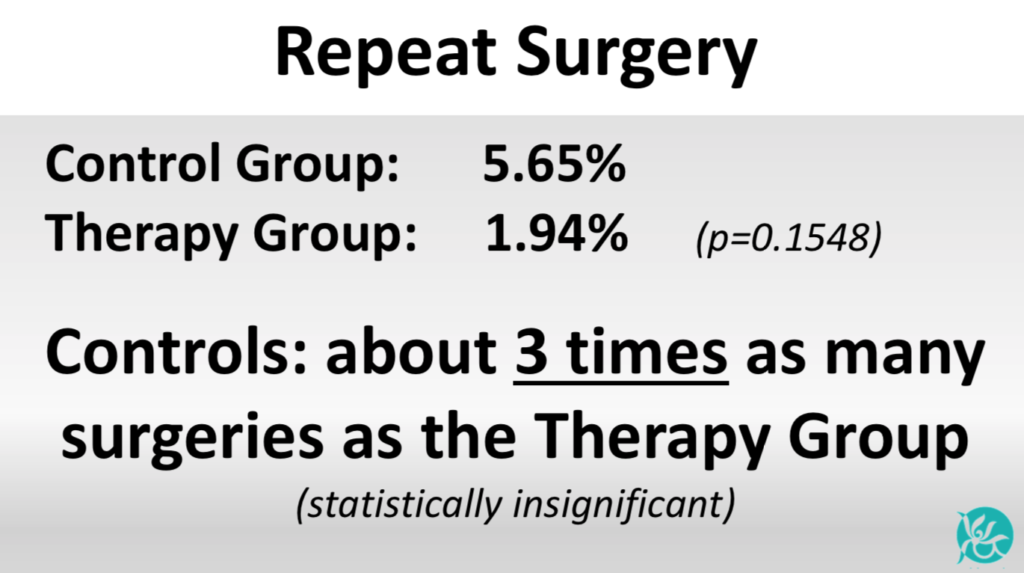
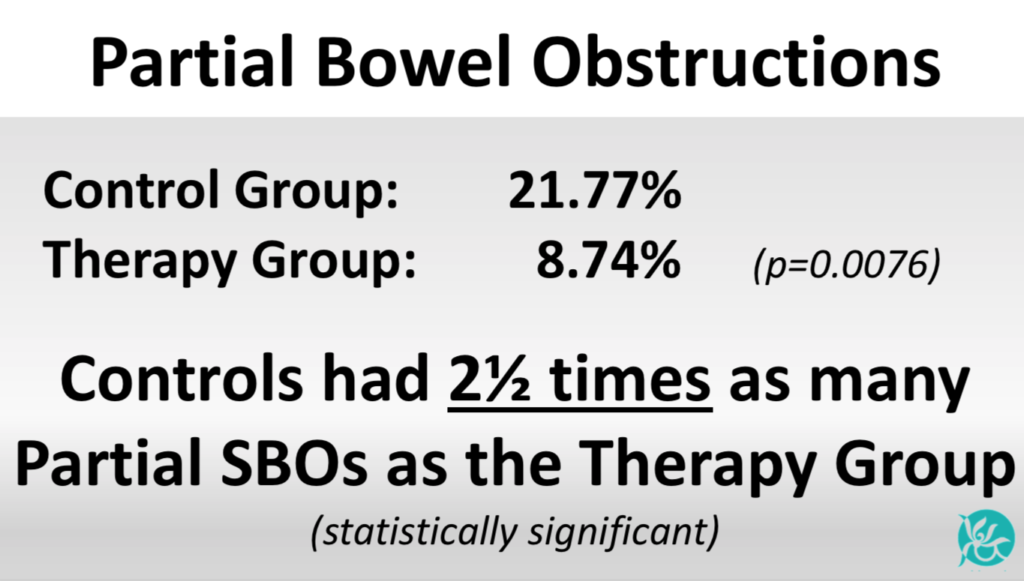
The same surgeons (both familiar with our work) also co-authored a Controlled Phase Two study which published in the World Journal of Gastroenterology the same month, examining patients with recurring bowel obstructions. That study addressed the difference between a Control Group who did not receive therapy (which is the norm) and a Therapy Group, which received the Clear Passage Approach. Among other findings, 15% of the Control Group had another total bowel obstruction within 90 days after the study ended compared to 1% of the group that received therapy. Detailed results are shown below:
This is considered a major Phase Two study. Below, we will take an in-depth look at the data – before and after the 90-day run of the study.
The Control Group (without CP therapy) had far less complex histories compared to the CP Treated Group. The authors stated that one would have expected worse results with the CP Treated Group. Here are the two groups as they entered the study:
Before CP TherapyAverage Age Controls: 36.4 + 12.5 years Therapy: 54.5 + 15.7 years (p<0.001) significant CP Therapy group averaged 18 years older Prior Surgeries Controls: 2.07 + 1.29 Therapy: 4.56 + 2.86 (p=0.0001) significant CP Therapy group: Over twice as many prior surgeries Years Impacted by SBOs Controls: 5.5 + 7.2 Therapy: 10.7 + 11.2 (p=0.0001) significant CP Therapy group: Twice the years impacted by obstructions Prior Partial SBOs Controls: 1.88 + 1.60 Therapy: 3.97 + 5.99 (p=0.0001) significant CP Therapy group: Twice as many partial obstructions Prior Total SBOs Controls: 2.17 + 1.85 Therapy: 1.68 + 7.95 (p=0.4894) not significant CP Control Group: Slightly more total obstructions; the statistician judged this insignificant | After CP TherapyPartial Bowel Obstructions Control Group: 21.77% Therapy Group: 8.74% (p=0.0076) significant Controls had 2½ times as many partial obstructions as the Therapy Group Total Bowel Obstructions Control Group: 14.52% Therapy Group: 0.97% (p=0.0003) significant Controls had 15 times as many total obstructions as the Therapy Group Repeat Surgery Control Group: 5.65% Therapy Group: 1.94% (p=0.1548) judged not significant Controls had 2.9 times as many surgeries as the Therapy Group |
Earlier Studies
2008 – First SBO Patients Treated
When published studies showed we could open fallopian tubes blocked by adhesions, we developed therapy to clear the adhesions that cause bowel obstructions. Our success with these patients came quickly, inspiring us to begin to track data suitable for publication.
2013 – SBO Published
We began publishing case studies about clearing bowel obstructions and adhesions via manual therapy using objective reports from independent physicians noting:
- Before and after x-rays showing cleared bowel obstruction;
- Before and after x-rays showing eliminated stricture (narrowing) in the bowel;
- A patient whose only nutrition was intravenous before therapy could eat normally following therapy.
2014 –Validated Measurement Test Published
Some patients who have recurring SBOs have other symptoms; others do not. We published a scientifically validated questionnaire to measure common but serious quality of life issues for patients experiencing small bowel obstructions ‘before and after’ therapy. This test, now available to all physicians and scientists, helped give an overview of ‘quality of life’ changes for people who suffer repeat obstructions.
2015 – Measuring and Publishing Data on Quality of Life After Therapy
The independent data noted above generated interest in further studies. Subjective data, such as pain relief, is considered relevant when screened using a scientifically validated test, such as the one we published in 2014. We use it to measure:
- Pain presence
- Pain severity
- Gastrointestinal symptoms
- Diet
- Medication
- Quality of life
- Range of motion (prior surgical adhesions can bind the abdomen, restricting trunk mobility)
As a result, we can now identify the areas where we are most effective, shown below.
2015 – Present Data to 15,000 Physicians
We were invited to present our work to 15,000 international gastroenterologists at Digestive Disease Week in Washington D.C. Results of that pilot study were published in the journal Gastroenterology (May 2015). Scientists noted improvement in every domain of ‘quality of life’ measurable for patients with prior bowel obstructions, including:
- Pain decreased in 85% of patients;
- Gastrointestinal symptoms deceased in 73% of patients;
- Diet improved for 100% of patients who reported a severe impact on their diet before therapy, and in 50% of patients overall;
- 83% of patients who were taking medication for bowel function maintenance before therapy were able to completely stop their medication;
- Significant improvements in all six areas of trunk range of motion (flexion, extension, right and left side bending, right and left rotation)
Measuring Repeat Surgeries with and without Therapy
A vital concern for anyone who has ever undergone the terrible ordeal of bowel obstruction surgery is to avoid repeat hospitalization and surgery. Adding to this concern is the fact that abdominal surgery is the primary cause of bowel obstruction. Thus, post-surgical SBO patients worry they will have to undergo one or more repeat surgeries, leaving them in a cycle of obstruction-surgery-adhesions with no end in sight.
We have treated over 350 patients over the last eight years with concerns they would have to undergo another obstruction surgery. This large number allows us to start gathering long-term data on success rates, including percent of return surgeries in our patients compared to those who don’t receive our therapy.
We compiled the first of our long-term “return to surgery” rates from two sets of patients who received our therapy, and compared them to the norm (no therapy):
- Dataset #1 – Clinical data on our earliest bowel obstruction patients
- Dataset #2 – Scientific data published in a 2015 medical textbook
Repeat Surgeries without CPA Therapy
Repeat surgery within 30 days: According to U.S. government statistics, 18% of patients who undergo bowel obstruction surgery are readmitted to the hospital within 30 days after their surgery. Some of these repeat surgeries are due to infection from bowel contents that leaked into the abdominal cavity during the first surgery. Set free in a warm, dark, moist environment, the escaped bacteria can grow quickly, creating an internal infection that requires immediate repeat surgery, with antibiotics administered directly to the surgical site.
Repeat surgery within two years: Abdominal surgery is the primary cause of small bowel obstruction. Based on medical literature, the expected rate of repeat surgery after SBO surgery is 30% without therapy; repeat surgeries generally start within the first two years.
Repeat Surgeries with CPA Therapy
Dataset #1 – Initial Data
Repeat surgeries up to five years after therapy: Initial clinical data examines our first 69 Clear Passage bowel obstruction patients for up to five years (mean 2.2 years) after therapy in two areas:
- Repeat surgeries with and without compliance with our home program
- Conditions where we observed negative outcomes
In this Dataset, 7% of patients we treated who followed our home program required additional surgery after therapy – much better than the 30% rate without Clear Passage therapy. In examining the unsuccessful cases, we were able to identify factors that pre-dispose a person to negative outcomes – to improve our results.
While our initial results with therapy were several times better than surgery, we continued to improve upon them over the years, as we modified our therapy, introduced a home maintenance program, and screened better for patients we felt would not benefit our treatment.
Dataset #2 – Published Results
Repeat surgeries after therapy:
As our inquiries became more scientific, we created and published a validated test to get a broader view of our results. This test gave more definitive scientific results, which were published in the medical textbook “Intussusception and Bowel Obstruction” (Rice & King, 2015). This Dataset showed a 3% return for surgery in bowel obstruction patients up to 35 months (mean 19 months) after therapy. Based on medical literature, the expected rate for return surgery would have been 30% – ten times our number.
Conclusion: A Chance to Avoid Surgery
Whether our “return to surgery” rate is 7% or 3% or between the two, it is clear that we greatly improved on the 30% “surgical return rate” for patients who do not receive our therapy. As we near the end of our first decade of treating patients with recurring bowel obstructions, we assume our rates will remain stable — or improve.
Pre-Disposing Factors for Poor Results
Over the years, we have learned to screen for conditions that pre-dispose a person to negative results. Thus, we now examine each patient’s medical history for present or past conditions that could lead to negative outcomes, e.g. active infection, radiation enteritis (bowel inflammation due to radiation therapy for cancer) and uncontrolled inflammatory processes (e.g. Crohn’s disease uncontrolled by medication). To help our patients, we now delay or decline applicants with conditions that could lead to negative outcomes. Please consult us if you have concerns about possible contraindications.
Life After Therapy
If you have undergone bowel obstruction surgery, your intestines have been structurally compromised. It is impossible to return the internal abdominal structure you had before your first surgery. We cannot guarantee you will be able to eat all of the foods you ate before you began having obstructions. Some patients do; some do not.
Nevertheless, it is clear from the numbers above, and responses from the 400+ SBO patients we have treated to date, that the benefits of therapy and our home maintenance program are significant for most patients. The success rates of our therapy in eliminating the need for surgery and restoring quality of life are very encouraging.
Future Studies
We continue to follow our patients over time and collect outcome data, both long term and immediately following treatment. It is worthy to note that the initial results from the 400+ patients for whom we are presently gathering follow-up are equal or better than the numbers in the 69 patients above.
Background
At Clear Passage®, we have always been cautious about keeping patients safe, and making claims about our results. After we opened our first fallopian tubes in 1989, we spent 30 years studying adhesions, refining treatment techniques, having biostatisticians calculate what techniques worked best, further refining, and then publishing our results.
In 2008, we turned our attention to clearing larger tubes – intestinal blockages. This page traces much of our history clearing small bowel obstructions from the beginning to the present.
Program and Results
We do not have privileges at your hospital. Our program is designed to clear blockages at our facilities and prevent recurrences. Our most current success rates for preventing recurring bowel obstructions and repeat bowel surgeries is shown below. This data has been verified in a peer-reviewed, controlled study co-authored by physicians from Harvard, Stanford, and Washington University medical schools.
Rounded to the nearest numbers (exact numbers and p-values further down this page) our most current results can be summarized:
We decrease recurring total bowel obstructions by 15 times the norm.
We decrease recurring partial bowel obstructions (hospitalization without surgery) by 2.5 times the norm.
We decrease repeat surgeries to the bowel by 3 times the norm.
Who Can Perform this Therapy?
Manual therapy to the bowel should be undertaken with caution. It should only be performed by therapists who are highly educated and knowledgeable treating the areas that contain the abdominal and reproductive organs. So many complex processes occur in the abdomen every day that treatment should be approached with caution, and a good understanding of the ramifications of applying pressures to various areas.
Elements of Our Bowel Obstruction Program
The years we have spent studying our techniques and results have helped us develop very clear elements for our programs, including
- Cautions and contraindications to manual therapy in the abdomen;
- Thorough Initial Evaluation and daily written reports for each patient;
- Exclusive manual techniques found to be safe and effective treating intestines;
- Oral and written patient education and home program designed to maximize long-term results.
Two educational goals for all patients include:
- Learning why and how adhesions form in the abdomen, and how to slow or prevent their formation, and
- Understanding how to maintain and even improve upon gains we give them during their 20-hour therapy protocol.
The following paragraphs and illustrations trace our history of learning to clear intestinal obstructions and return patients to a much higher quality of life. They also give an in-depth understanding of the best scientific data we have gathered on treating bowel obstructions since 2008.
History
Following the ‘scientific method’ for investigating new modalities, we began by publishing some remarkable case studies, all of which can be read at our Published Studies page. These studies included a woman who managed to stay alive despite a bowel that was totally blocked. When she arrived for therapy, her only nutrition was by intravenous PICC line. After several hours of our therapy, her physician was able to remove her PICC line – because she could eat normally. This and other surprising results inspired us to investigate further, with more involved studies.
Measuring Success
Due to the complex structure and functions of the bowel, measuring success for patients with recurring small bowel obstruction (SBO) presented opportunities and challenges. We found three major areas of concern that we could measure by comparing conditions before and after therapy:
- Structure – Independent radiographic images taken before and after therapy
- Repeat Events – Number of repeat obstructions before and after therapy
- Quality of Life – Graded by patients, results tabulated by biostatisticians
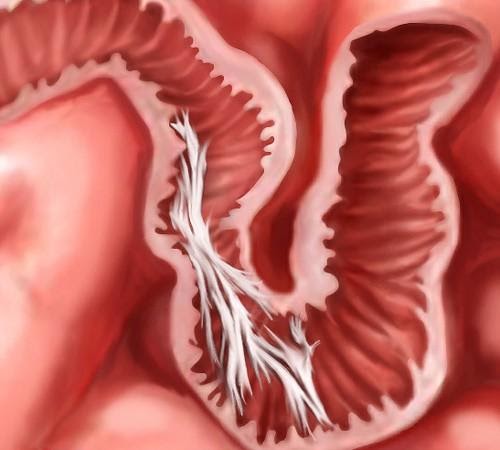

Structure – Before and After X-Rays
We found we could document the structure of intestines in patients who had “small bowel follow through” test (SBFT) before and after therapy. In this test, our patient would swallow a cocktail that contained a barium ‘tracer’ that would give precise x-ray images of the interior of the bowel. Concerned that they might obstruct from the test, many patients avoided taking this test which involves swallowing a rather thick liquid containing radio-opaque barium. Nevertheless, the test gives a good picture of the inside the bowel; it can show where narrowing or obstructions occur. Using this test, we’ve been able to get some very clear images that document bowel obstructions in patients who arrive for therapy – and the result of our hands-on care on their previously blocked intestines.
In the images shown here, one can clearly see the progress of the liquid (shown in white) as it passes through the small intestine, and where it becomes blocked.
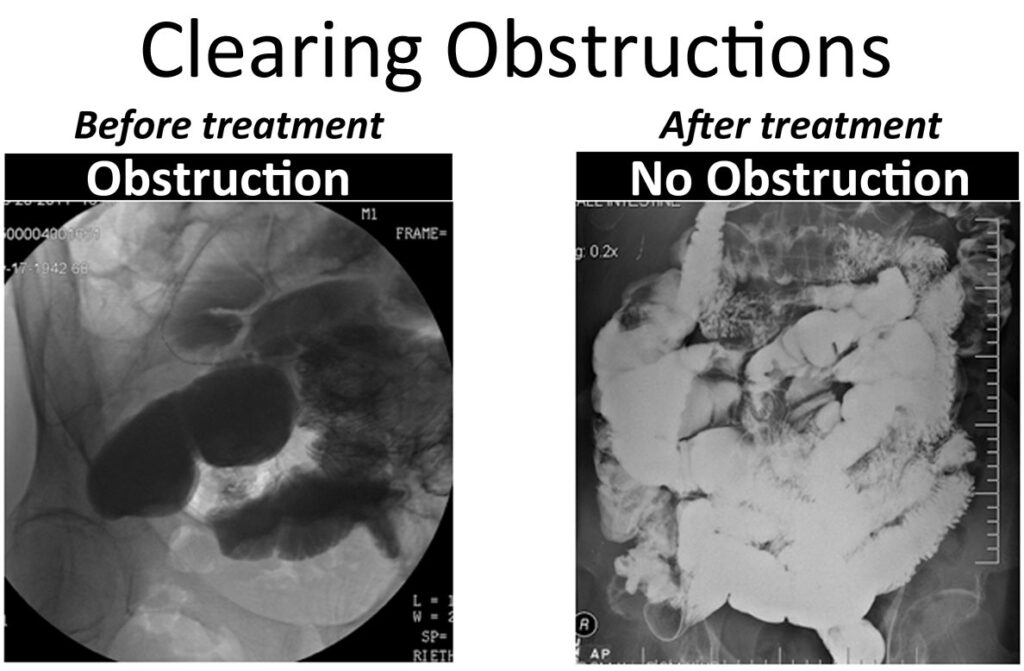
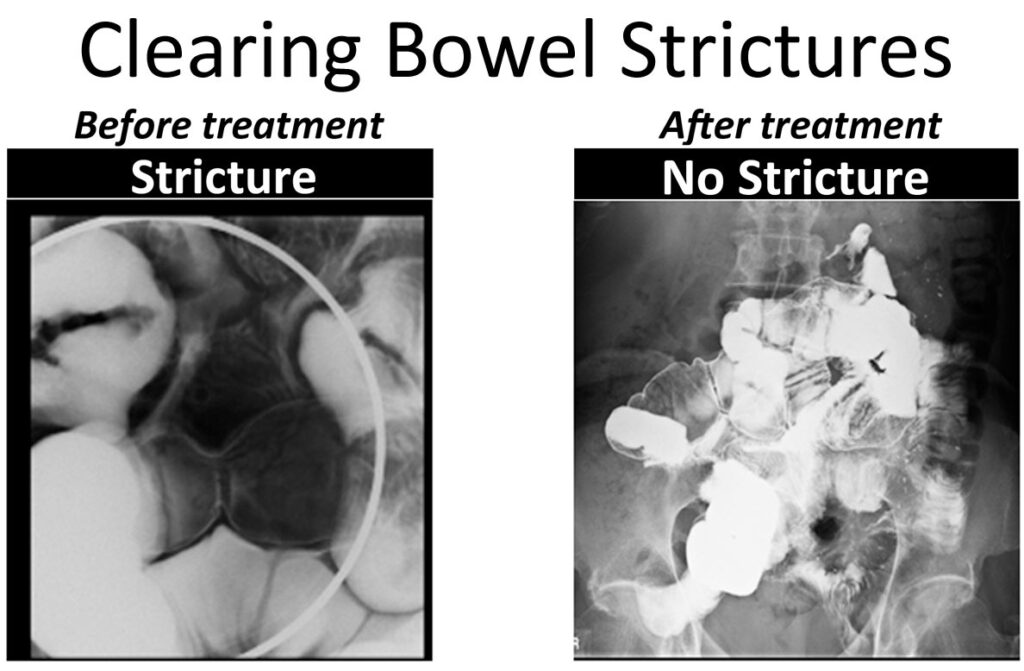
Clearing Bowel Obstructions
These images give dramatic testament to the positive changes you can actually see, in ‘before and after’ images:

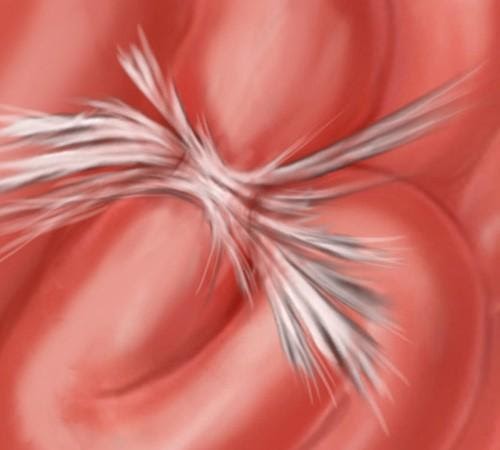
In the two-part image shown here, we see in the image taken “Before” therapy, an hourglass-shaped stricture (narrowing) is visible in this patient’s intestines. The constriction is so significant that very little dye goes through to the bowels below – beyond the stricture. This patient was scheduled for emergency surgery before we treated her. Instead, she decided to try Clear Passage® therapy first.
Comparing that with the “After” image, we can clearly see that the stricture completely resolved (disappeared) after therapy designed to clear adhesions from the area. Notice also how open the intestines are above and below the site of the prior stricture in the areas beyond the previously narrowed bowel. The radiologist cited this a “normal bowel” after therapy, so the surgeon canceled the planned surgery.
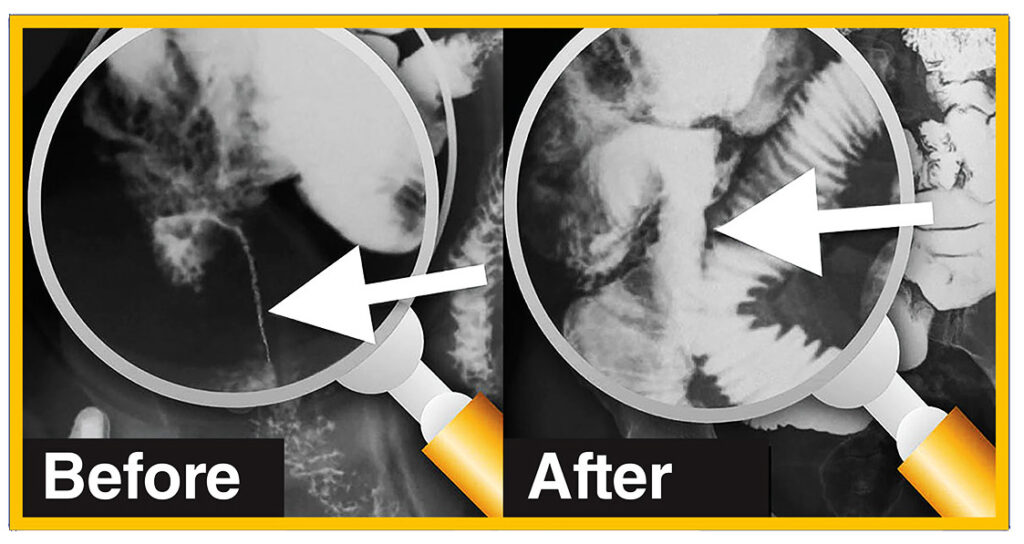
In this second set of images, we see a very dramatic string stricture “Before” therapy. This is a 3-inch long section where the contents of the bowel are passing through an area that is narrowed to the size of a coffee straw. Certainly, no food was going to pass through this area. No dye is seen passing through other loops of the bowel beyond the stricture. Again, this patient opted to first try Clear Passage® therapy, rather than undergo abdominal surgery to repair her bowel.
In the image taken “After” therapy, we can see that the area that was once so narrow for its entire length has broadened dramatically. In fact, this radiologist noted after therapy “this patient now has a normal bowel.” Dye is flowing easily into other bowel loops after treatment. Again, the surgeon canceled the planned surgery.
While we have published similar “before and after” images, these are clear and demonstrative. Once thought impossible, these films objectively show the effectiveness of our manual therapy, designed and tested for its ability to decrease adhesions and dramatically improve the structure of the bowel.
Repeat Events – Decreasing Recurring Obstructions
Surgery as a Cause of SBO
It is a well-known fact that surgery is the primary cause of bowel obstruction. No matter how compassionate, brilliant or skilled the surgeon, the body must heal from the cuts or burns imposed by the surgery. The first step in the process of healing from surgery is the laying down of adhesions (scar tissue) in a random pattern over the tissue which has been damaged. Thus, the surgery designed to cure the obstruction can be the cause of the next obstruction.
Surgery as a Cause of SBO
In some cases, a drop of bacteria-laden bowel contents can leak unseen into the abdomen before the physician closes the patient. Set free in this warm, moist and dark environment, bacteria can proliferate quickly. Perhaps for that reason, roughly one in five (18 % per HHS) of all bowel resection patients are readmitted to the hospital within 30 days of their SBO surgery, often for peritonitis or other
infection that occurs when bacteria freed from the intestine spread throughout in the post-surgical abdomen. In this case, the physician will often reopen the patient surgically to introduce antibiotics directly into the infected spaces. The surgeon may choose to leave the body open to continue to administer medications directly into the abdomen and allow scarring to occur from the inside out to treat all of the infection. Naturally, this tends to create even more adhesions.
Even for those who are not re-admitted to the hospital during the month after surgery, the chance of a repeat obstruction caused by a prior surgery are too high. While surgery is routinely cited as the primary cause of bowel obstruction, a recent study in the Journal of the American Medical Association[i] notes that bowel resection is the 2nd most common emergency surgery in the U.S.A. and carries the highest complication rate (47%). Deaths from emergency surgery were up to 8 times more likely than the same procedure done electively.
Measuring Repeat Obstructions
Most of our SBO patients are too familiar with the problem of repeat obstructions. They come to us with the goal of “no more obstructions.” They tell us they are tired of a lifetime of wondering “Is this the day I’m going to die?” or “Is this the day I’m going to have to be struck down with severe pain and have to go to an emergency room with an obstruction?” Our patients ask us their chance of avoiding future obstructions so they can get back to living their lives without dread or uncertainty. In order to give a truthful answer, we put this question to our research staff.
We enlisted the guidance of physicians and researchers from several medical schools including Harvard, Stanford, Washington University, the Universities of Florida and of Arizona. They helped design a controlled study of 239 patients who were experiencing recurring bowel obstructions. Our job was to treat about half of them and compare results to untreated patients.
We treated 103 of the patients (the Therapy Group) and did not treat 136 of them (the Control Group.) The typical Therapy patient received our usual protocol: 20 hours of Clear Passage® treatment over 5 days. Control patients received the present Standard of Care – which is no therapy. We measured repeat Total and Partial Obstructions and Repeat Surgeries 90 days after the study closed.
Results (shown here) were remarkable.
The group we did not treat had 15 times more total bowel obstructions than those we treated. In fact, less than 1% of the patients we treated underwent another total bowel obstruction measured 90 days after the study closed. By contrast, close to 15% of the Controls (no therapy) had another total obstruction within the same 90-day period. Measured in both statistical and humanitarian ways, we found these results to be wonderful.
As shown in these images, the untreated group also had 2½ times more partial obstructions and 3 times as many surgeries as the patients we treated.
Improving Quality of Life
Quality of Life is an important measure of success for patients who have undergone the trauma of bowel obstruction (with or without surgery), followed by years of fear of having another one – or more. So many of these patients are miserable, often in pain; frustrated with a medical system they feel has let them down. Many report that their physicians say “there’s nothing you can do to change this.” Virtually all of these people live in fear of another obstruction that could happen at any time. We are glad that our therapy is beginning to turn that attitude around.
We hired a biostatistician to design, validate and publish a questionnaire and rating tool to measure quality of life in the five major ‘domains’ where our SBO patients report problems:
- Diet
- Pain
- Medication
- Quality of Life Issues, and
- Gastrointestinal (GI) Symptoms
The questionnaire was given to patients when they enrolled in the study, then again 90 days after the study closed. The biostatistician was able to measure changes (if any) between the start and end dates for both the Therapy and the Control Group.
Realizing that both the degree of pain and the ability to move freely affect Quality of Life, we added a “pain rating” section, and a section that compared ‘before and after’ Trunk Range of Motion for each participant.
- The Diet Domain assessed the diet of the subject from inability to tolerate any liquid to a normal solid food diet.
- The Pain Domain reported pain throughout the body, with oral intake of food or liquid, and with bowel function.
- The Gastrointestinal (GI) Symptom Domain quantified symptoms often associated with SBO such as nausea, emesis, bowel spasm and constipation.
- The Medication Domain reports the frequency of medications required to maintain bowel function.
- The Quality of Life Domain quantified the amount of time off work and social activities. In addition, it quantified each patient’s overall concern regarding their bowel function. We found that all of these tend to be major lifetime concerns for many people who experience recurring bowel obstructions.
- Trunk Range of Motion measured any increase in Range of Motion of the trunk after therapy.
Quality of Life – Statistically Measured Results
A Note on Statistics
Statisticians measure results by asking “what is the chance this result could have occurred by chance?” In this study, they used the common statistical measure (p=.05). This means if the measure is smaller than “5 out of 100”, the result is statistically significant (reliable). Any number greater than “.05” is considered clinically insignificant (unreliable). The data in the controlled study shown here, and published in the prestigious World Journal of Gastroenterology, showed very high statistical significance (reliability) at p<0.0001. Thus, the chance the numbers are unreliable was less than 1 out of 10,000 for Clear Passage® patients in the domains shown below. In essence, these results are considered highly reliable.
Trunk Range of Motion measurements showed that every Clear Passage® patient demonstrated improvement in Range of Motion (p<0.0001) extrapolated statistically in the table to the right.
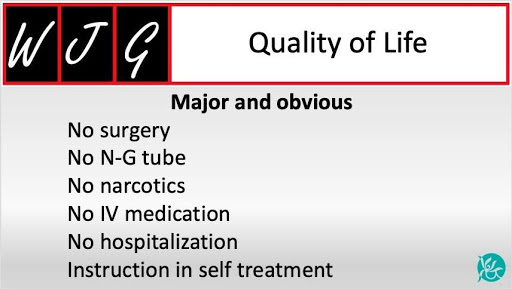
In addition to the statistical measures shown above, the journal notes or implies other major or obvious Quality of Life advantages of Clear Passage over the present Standard of Care (no therapy). These tend to include hospitalization, insertion of an NG tube, intravenous hydration, possible surgery, and ongoing fear of another obstruction. (The difference in this fear was significant in the Quality of Life domain.) These “other advantages” are shown here in an image labeled Quality of Life.
Results (direct quote from the study)
Despite histories of more prior hospitalizations, obstructions, surgeries, and years impacted by bowel issues, the 103 CP-treated subjects reported a significantly lower rate of repeat SBO than 136 untreated controls (total obstructions P = 0.0003; partial obstructions P = 0.0076).
Subjects treated with the therapy demonstrated significant improvements in five of six total domains in the validated Small Bowel Obstruction Questionnaire (SBO- Q).
Domains of diet, pain, gastrointestinal symptoms, quality of life (QOL) and pain severity when compared to post CPA treatment were significantly improved (P < 0.0001).
The medication domain was not changed in the CPA treated group (P = 0.176).


