“PCOS is a common hormonal disorder affecting women of reproductive age. It is characterized by a combination of symptoms that can significantly impact a woman’s physical and emotional well-being.”
Common Symptoms
PCOS symptoms, often stemming from hormonal imbalances (high androgens) and insulin resistance, commonly include irregular or missed periods, excess body/facial hair (hirsutism), severe acne, and difficulty losing weight. Other symptoms include hair thinning on the scalp, skin tags, and darkened skin patches.
Other Associated Symptoms
Beyond the primary indicators, other symptoms are commonly linked with PCOS, impacting various aspects of health. These can include metabolic issues, mental health challenges, and sleep disturbances, all requiring attention for comprehensive management.
Metabolic Disturbances and Insulin Resistance
People with PCOS may experience insulin resistance, where their body’s cells don’t respond to insulin effectively. This often leads to elevated insulin levels, increasing the risk for type 2 diabetes and heart disease. Up to 80% of women with PCOS face this challenge.
Psychological Impacts and Mood Disorders
Many women with PCOS report significant psychological distress. Women with PCOS may experience depression, with symptoms up to three times higher than in the general population. Anxiety is also common, with some studies showing rates up to six times greater.
Living with PCOS can be an emotional journey, impacting overall well-being. The chronic nature of symptoms like acne, unwanted hair growth, and weight fluctuations can understandably contribute to feelings of self-consciousness or frustration. Managing these symptoms and the associated health risks often requires ongoing effort, which can be mentally taxing. Support systems and mental health resources are available to help you navigate these challenges.
Sleep Apnea and Fatigue Patterns
Struggling with sleep apnea, a condition where breathing repeatedly stops and starts during sleep. This often results in chronic fatigue and daytime sleepiness, affecting the energy levels and daily functioning.
The link between PCOS and sleep apnea is complex, but it is often attributed to hormonal imbalances and obesity, both common in women with PCOS. Untreated sleep apnea can worsen insulin resistance and contribute to cardiovascular problems, forming a cycle of health challenges. Addressing sleep disturbances is an important step in improving overall health and quality of life when managing PCOS.
KEY FACTS & STATISTICS
- PCOS affects an estimated 10–13% of reproductive-aged women globally. Some sources indicate a range of 5-13% or 6-13% worldwide. In the US, it affects about 1 in 10 women of childbearing age, or 5 to 6 million women.
- Up to 70% of women with PCOS worldwide may be undiagnosed.
- From 1990 to 2021, global PCOS cases increased by 56% (incidence), 59% (prevalence), and 58% (Disability-Adjusted Life Years – DALYs) among females aged 10-24. The age-standardized incidence rate rose from 49.45 to 63.26 per 100,000.
- Projections indicate a continued increase in global PCOS incidence by 8.32% by 2036.
- PCOS is the most common cause of anovulation globally and a leading cause of infertility.
- Approximately 65-80% of women with PCOS experience insulin resistance, independent of obesity.
- 50% of women with PCOS will become diabetic or pre-diabetic before age 40.
- The prevalence of depressive symptoms is up to three times higher, and anxiety symptoms are up to six times higher in patients with PCOS.
EXPERT INSIGHTS
- Dr. Jessica Chan, an assistant professor of Obstetrics and Gynecology at Cedars-Sinai and a reproductive endocrinologist, states that PCOS is a set of symptoms resulting from a problem with reproductive hormones that can lead to irregular periods, excess hair growth or acne, and infertility. She emphasizes that while there’s no cure, symptoms can be managed through each stage of the disorder.
- Dr. Itunu Johnson-Sogbetun, a Family Physician specializing in women’s health, highlights that PCOS is a whole-body hormonal disorder and not just a reproductive condition, despite its name. She notes its impact on insulin resistance, increasing the risk of diabetes and heart disease, and also affecting mental health.
- Dr. Pardis Hosseinzadeh, fertility specialist and PCOS advocate, and Sasha Ottey emphasize the long-term health implications of PCOS, including increased risk of type 2 diabetes, metabolic syndrome, abnormal lipids, chronic hypertension, early-onset cardiovascular disease, non-alcoholic fatty liver disease, sleep apnea, and precancerous lesions of the uterus.
The Role of Mechanical Adhesions in Pelvic Health
Understanding the body’s interconnectedness can illuminate new pathways for managing PCOS. Mechanical adhesions, often microscopic, can restrict organ movement and blood flow in the pelvic area, potentially contributing to discomfort and dysfunction. Addressing these adhesions may improve overall pelvic health.
Integrated Holistic Approaches to Hormonal Balancing
Managing PCOS requires a comprehensive strategy that addresses the disorder’s multifaceted nature. Combining conventional treatments with lifestyle adjustments and complementary therapies can offer a more holistic path to hormonal balance.
This integrated approach acknowledges that PCOS is more than just a reproductive issue; it is a whole-body hormonal disorder. Better outcomes are achieved by combining dietary changes, structured exercise, and behavioral interventions with medical treatments. This synergy can help regulate insulin levels, reduce androgen production, and alleviate symptoms like irregular periods, acne, and excess hair growth, improving overall well-being.
Clear Passage® Method for Reproductive Wellness
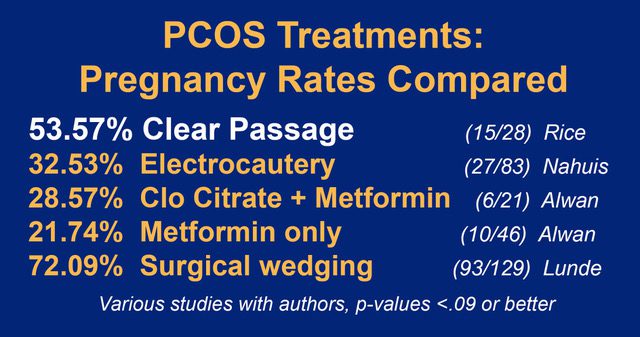
Consider the Clear Passage® Method, a specialized manual physical therapy, as a non-surgical option. This therapy focuses on detaching adhesions to restore mobility and improve blood flow, offering a potential benefit for reproductive health and symptom management in women.
The Clear Passage® Method works by gently breaking down adhesions, which are often microscopic and can bind tissues together, restricting natural movement and function. This targeted therapy aims to enhance organ mobility and improve circulation within the pelvic region. For those with PCOS, this can mean reduced pain, improved menstrual regularity, and potentially increased fertility by optimizing the environment for reproductive organs.
TRENDS & DEVELOPMENTS
- Increased incidence among younger individuals: A recent study showed increased rates of PCOS diagnoses among individuals aged 16 to 20 years in 2019 compared to 2006 in the US.
- Integrated care: There is a desire among women with PCOS for more integrated clinics offering a “one-stop” solution, combining conventional treatments with lifestyle counseling and complementary therapies.
- Cardiovascular disease risk: PCOS is increasingly recognized as a cardiovascular disease risk-enhancing factor, with evidence for increased risk of myocardial infarction and stroke even in reproductive years.
- Gut microbiome research: Novel insights into alterations in the gut microbiome in PCOS suggest possible contributions to metabolic dysfunction and inflammation, opening avenues for innovative therapeutic strategies. This gut dysbiosis may also be linked to the high prevalence of mental health disorders like depression and anxiety in PCOS.
- Early diagnosis and prevention: Given the increased prevalence of multisystem comorbidities, early diagnosis, especially in adolescence, is crucial for appropriate counseling, early prevention, and frequent cardiometabolic screening.
- Machine learning for diagnosis: Researchers are exploring machine learning algorithms from electronic health records to predict PCOS diagnosis, aiming for more timely diagnosis and optimized referrals.
Advances in Non-Invasive Therapeutic Interventions
Scientists are exploring innovative non-invasive approaches to manage PCOS, moving beyond traditional methods. New research focuses on therapies like the therapy that Clear Passage® provides, which minimize discomfort and recovery time for individuals.
Modern Nutritional Science for Endocrine Support
Recent discoveries in nutritional science offer targeted support for endocrine balance in PCOS. Dietary interventions are being refined to address insulin resistance and hormonal dysregulation effectively.
Understanding the impact of diet on the endocrine system is becoming increasingly refined. Specific nutritional strategies, such as low-glycemic index diets and the Mediterranean diet, are demonstrating significant benefits in managing PCOS. These approaches can help stabilize blood sugar, reduce insulin levels, and potentially lower androgen production, directly addressing some of the core hormonal imbalances you might experience with PCOS.
Telemedicine and Digital Health Monitoring Tools
Digital health solutions are transforming PCOS management, offering remote monitoring and virtual consultations. These tools provide convenient access to care and empower individuals to track their health metrics.
The convenience of telemedicine and digital health monitoring tools is reshaping how you can manage PCOS. Expert advice and ongoing support are now available from the convenience of home. These platforms allow for continuous tracking of symptoms, medication adherence, and lifestyle changes, providing the healthcare provider with valuable data to create a personalized treatment plan and ensure consistent care.
PRACTICAL DATA
- Lifestyle modifications: Dietary changes, structured exercise programs, and behavioral interventions are considered first-line management, especially for overweight and obese women with PCOS.
- Dietary interventions: Low-glycemic index (low-GI) diets and the Mediterranean diet are widely studied for their ability to promote weight loss, lower insulin levels, and reduce androgen production.
- Weight loss: Even a small amount of weight loss (5-10% of overall weight) can help overweight women with PCOS begin ovulating on their own.
- Treatment tailoring: No single treatment can reverse all hormonal changes or address all clinical features of PCOS; therefore, medical management should be tailored to individual symptoms.
- Metformin: In combination with a combined oral contraceptive pill, metformin may benefit high metabolic risk groups, including women with a BMI >30 kg/m², diabetes risk factors, and/or impaired glucose tolerance.
- Regular periods: Women with PCOS should aim for a period at least once every three months due to the risk of endometrial hyperplasia or endometrial cancer.
- Clear Passage® Therapy: Systematic releasing of adhesions that bind the ovaries and uterus may help hormones and impact fertility.
Approaching PCOS management, various practical strategies can significantly alleviate symptoms. Focusing on lifestyle modifications, tailored medical treatments, and understanding different management approaches.
Symptom Severity Scoring Systems
Assessing the impact of PCOS symptoms helps in customizing a treatment plan. These systems provide a structured way to track changes and evaluate the effectiveness of interventions over time.
Comparison of Pharmacological vs. Holistic Management
Considering individual symptoms is key, as no single treatment addresses all aspects of PCOS. Medical management should be tailored to the patient’s specific needs, combining different approaches for optimal results.
When comparing different management strategies, you will find that pharmacological interventions often target specific symptoms, such as metformin for insulin resistance or birth control for regulating periods. Holistic approaches, including dietary changes and structured exercise, are considered first-line management, especially for weight management and overall metabolic health. The table below outlines key differences:
PCOS Management Approaches
Pharmacological Management
- Uses medications like Metformin or combined oral contraceptive pills.
- Targets specific hormonal imbalances or metabolic risks.
- Often tailored for high metabolic risk groups.
Holistic Management
- Focuses on lifestyle changes: diet, exercise, behavioral interventions.
- Aims for overall well-being, weight loss, and reduced androgen production.
- Includes low-GI diets, the Mediterranean diet, and regular physical activity.
COMMON MISCONCEPTIONS
Myth: PCOS only affects overweight women.
Fact: PCOS can affect individuals of all shapes and sizes, including those with a normal or low BMI. While weight gain is a symptom, it’s not a prerequisite for diagnosis.
Myth: If you have regular periods, you don’t have PCOS.
Fact: Even people with regular periods can have PCOS. Menstrual irregularities are just one of many possible symptoms.
Myth: People with PCOS cannot get pregnant.
Fact: While PCOS can make conception more difficult, many individuals with PCOS can and do get pregnant with the right treatment, like the one that Clear Passage® provides and supports, including lifestyle changes or medication.
Myth: Birth control is the only form of treatment.
Fact: While birth control can manage symptoms, PCOS treatment is often tailored and may include lifestyle changes, other medications, and fertility treatments; it is not a cure.
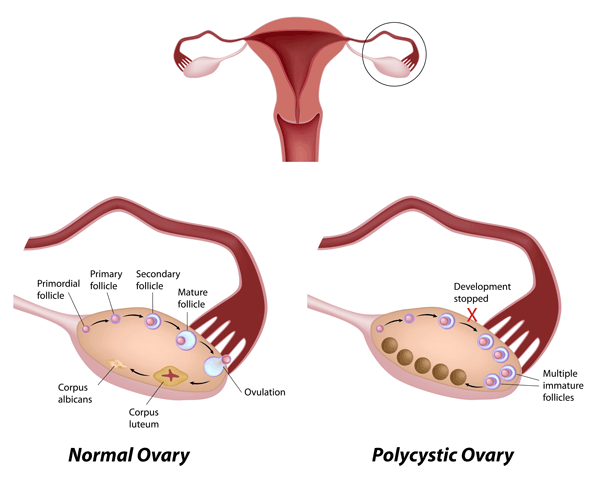
Myth: All women with PCOS have ovarian cysts.
Fact: The term “polycystic” refers to the appearance of multiple small follicles on ultrasound, not necessarily traditional cysts, and not everyone with PCOS will have them. The diagnosis requires at least two out of three criteria, which include irregular periods, hyperandrogenism, or polycystic ovaries on ultrasound.
Myth: PCOS is caused by poor lifestyle choices.
Fact: PCOS is a complex hormonal disorder influenced by genetics, insulin resistance, and inflammation; lifestyle factors can influence symptom severity but are not the root cause.
Understanding PCOS means dispelling common myths that often surround the condition. You might encounter misinformation about symptoms, diagnosis, and treatment, which can complicate the journey. This section addresses some widely held but incorrect beliefs.
IMPORTANT TERMINOLOGY
- Androgens: Often referred to as “male hormones,” females produce androgens, but women with PCOS often have higher levels, contributing to symptoms like acne and excess hair growth.
- Anovulation/Anovulatory cycles: Menstrual cycles where an egg is not released, leading to infertility. PCOS is the most common cause of anovulation.
- Hirsutism: Excessive hair growth in a male-pattern distribution (e.g., face, chest, back), a common symptom of high androgen levels in PCOS.
- Hyperandrogenism: The presence of high levels of androgens, either through elevated blood tests or clinical signs like hirsutism and acne.
- Insulin Resistance: A condition where the body’s cells don’t respond properly to the hormone insulin, leading to elevated insulin levels and increased risk for type 2 diabetes. It is common in women with PCOS.
- Oligomenorrhea: Infrequent menstrual periods.
- Polycystic Ovaries: Ovaries that appear enlarged with multiple small follicles on ultrasound. This is one of the diagnostic criteria for PCOS, but not all women with PCOS have them.
- Rotterdam criteria: Widely recommended diagnostic criteria for PCOS, requiring at least two of the following: irregular periods/ovulatory dysfunction, hyperandrogenism (clinical or biochemical), or polycystic ovaries on ultrasound.
Defining Hyperandrogenism and Hirsutism
Understanding these terms is key to recognizing PCOS. Hyperandrogenism refers to elevated androgen levels, seen in blood tests or through physical signs like acne. Hirsutism, a direct result of hyperandrogenism, describes excessive hair growth in areas typically associated with male patterns.
Understanding Luteinizing Hormone and FSH Ratios
Atypical ratios of Luteinizing Hormone (LH) to Follicle-Stimulating Hormone (FSH) often indicate PCOS. These hormones play a central role in the menstrual cycle. A higher LH:FSH ratio can disrupt ovulation.
The body produces both LH and FSH to regulate ovarian function and the menstrual cycle. In PCOS, an imbalance, specifically a higher LH relative to FSH, can prevent follicles from maturing properly and releasing an egg, leading to anovulation and irregular periods. This disruption is a key feature in many PCOS diagnoses.
A peer-reviewed study of 1,392 women conducted over ten years showed hormonal improvement in 49% of women diagnosed as infertile due to high FSH (follicle-stimulating hormone[i]) after receiving Clear Passage ® therapy. Over 39% of women diagnosed with FSH levels above 10 conceived after a 5-day Clear Passage® session; most had natural pregnancies.
Explaining Insulin Sensitivity and Glucose Tolerance
Insulin sensitivity and glucose tolerance are vital concepts when discussing PCOS. Insulin resistance, common in PCOS, means that the cells don’t respond effectively to insulin. This leads to higher blood glucose levels.
The body produces insulin to regulate blood sugar. When you have insulin resistance, the pancreas works harder, producing more insulin to try to maintain normal blood glucose. Over time, this can exhaust the pancreas and lead to impaired glucose tolerance, pre-diabetes, and eventually type 2 diabetes, a significant comorbidity with PCOS.
Diagnostic Criteria and the Rotterdam Consensus
Confirming a PCOS diagnosis relies on specific criteria, most commonly the Rotterdam Consensus. This internationally recognized guideline helps healthcare professionals accurately identify the condition. You will need to meet at least two of these criteria for a clinical diagnosis.
Requirements for a Clinical PCOS Diagnosis
To receive a PCOS diagnosis, you must exhibit at least two of the three Rotterdam criteria. These include irregular periods or ovulatory dysfunction, hyperandrogenism (clinical or biochemical), or polycystic ovaries on ultrasound. The doctor will assess the symptoms.
Differential Diagnosis to Rule Out Other Disorders
Physicians must exclude other conditions that mimic PCOS symptoms before making a definitive diagnosis. This process ensures that the patient will receive the correct treatment for their specific health needs. Ruling out other disorders prevents misdiagnosis.
The doctor will carefully consider other potential causes for the symptoms, such as thyroid disorders, congenital adrenal hyperplasia, or hyperprolactinemia. These conditions can present with similar signs, such as irregular periods or excess hair growth. A thorough evaluation helps distinguish PCOS from these other endocrine issues, ensuring appropriate management. This diagnostic rigor is vital for well-being.
The Importance of Comprehensive Blood Panels
Comprehensive blood panels are vital for evaluating hormone levels and metabolic health. These tests help confirm hyperandrogenism and assess for insulin resistance. They provide crucial insights into the internal physiological state.
Blood tests will specifically measure androgen levels, such as testosterone, and evaluate insulin sensitivity. These panels also screen for other metabolic markers, like lipids, which are often dysregulated in PCOS. This detailed blood work helps tailor treatment plans, addressing both hormonal imbalances and metabolic risks associated with PCOS, including the risk of type 2 diabetes.
Fertility Challenges and PCOS
Many women with PCOS experience difficulty conceiving, as the condition is a leading cause of infertility globally. Understanding the specific ways PCOS impacts the reproductive system can help you explore effective strategies for achieving pregnancy.
Anovulation and the Path to Conception
Irregular or absent ovulation, known as anovulation, is a primary barrier to conception for many with PCOS. The body struggles to release an egg consistently, making a natural pregnancy challenging without intervention.
Improving Egg Quality Through Systemic Health
Optimizing overall health can significantly impact the quality of eggs. Addressing underlying metabolic issues, such as insulin resistance, and adopting a nutrient-rich diet support healthier ovarian function.
Focusing on systemic health can directly enhance egg quality. For instance, managing insulin resistance, which affects 65-80% of women with PCOS, can lead to better hormonal balance. Implementing dietary changes, like a low-glycemic index or Mediterranean diet, and engaging in regular exercise are first-line management strategies that promote weight loss and reduce insulin levels, creating a more favorable environment for egg development.
Reducing Pelvic Adhesions to Support Ovarian Function
Sometimes, physical obstructions like pelvic adhesions can hinder ovarian function and egg release. It is speculated that a mechanical aspect of PCOS in some women is when the ovaries become covered with collagen fibers, the building blocks of adhesions. The Clear Passage® method reduces these adhesions to improve the chances of conception.
Pelvic adhesions, fibrous bands of scar tissue, can develop around the ovaries and fallopian tubes, potentially interfering with ovulation and egg transport. While not directly caused by PCOS, it is yet another symptom of PCOS; addressing existing adhesions can optimize the reproductive environment. Consulting with a healthcare provider to assess for adhesions and discuss potential interventions, such as specific physical therapies or minimally invasive procedures, could be a beneficial step in the fertility journey.
Long-Term Health Monitoring
Understanding the long-term implications of PCOS is important for well-being. This condition can increase the risk for various health issues, including type 2 diabetes and cardiovascular disease. Staying proactive with regular health screenings and tailored management strategies is key to mitigating these risks and maintaining overall health.
Cardiovascular Risk Assessment in PCOS Patients
The risk of cardiovascular disease is higher with PCOS, even in reproductive years. Regular assessments, including monitoring blood pressure and cholesterol, are important. Early identification allows for lifestyle adjustments and medical interventions to protect heart health.
Managing the Risk of Endometrial Hyperplasia
Irregular periods associated with PCOS can increase the risk of endometrial hyperplasia. Aim for a menstrual period at least once every three months. This helps shed the uterine lining, preventing abnormal cell growth.
Sustained periods without shedding the uterine lining can lead to a buildup of the endometrium, which is the inner lining of the uterus. This thickening, known as endometrial hyperplasia, can progress to precancerous lesions and, in some cases, endometrial cancer. Regular menstrual cycles, whether naturally occurring or induced by medication, are a protective measure against this risk. The doctor can discuss various options to achieve this, ensuring that uterine health is maintained.
Type 2 Diabetes Prevention Strategies
You face a significantly increased risk of developing type 2 diabetes before age 40. Focusing on preventive strategies is therefore critical. Lifestyle modifications, such as dietary changes and regular exercise, are often the first line of defense.
Maintaining a healthy weight through dietary interventions like low-glycemic index (low-GI) diets or the Mediterranean diet can significantly improve insulin sensitivity. Even a modest weight loss of 5-10% of your total body weight can help regulate insulin levels and improve ovulation. Your healthcare provider might also recommend medications like Metformin, especially if you have a higher BMI or other risk factors for diabetes, to help manage insulin resistance and reduce your diabetes risk.
Conclusion
In a nutshell, with this in mind, understanding PCOS symptoms is diverse, impacting reproductive health, metabolism, and mental well-being. Recognizing these signs allows the patient to seek a timely diagnosis and personalized management. Tailoring treatments, including lifestyle changes and medication, helps you effectively manage specific symptoms and improve overall health.


