Our Program Costs
Costs for the complete 20-hour therapy program featured in published studies and used to calculate most of our success rates start at $7,500, which is paid before therapy starts.
Abbreviated and extended treatment plans are available. We are out-of-network for most insurers; some reimburse all costs, some a portion; some none at all. You can learn more on our Insurance and Financing page.
This page is designed to help give you an objective comparison of value, risk, and general outcomes of our therapy compared to other treatment options.
Unlock the potential for non-surgical healing with Clear Passage Physical Therapy’s innovative approach – Request Information and schedule your Free Consultation today to explore how our expert therapists can help you avoid surgery, reduce pain, and improve your quality of life, then visit our Apply to Therapy page
Cost vs. Risk and Value
Direct Comparisons of Treatment Options
We believe that each patient should be knowledgeable about all their treatment options. Further, they should be a part of their personal medical team. It is wise to directly compare treatment options including the documented risks, side effects and success rates of your choices. To help you compare the value of the Clear Passage® Approach (CPA) to your other options, we offer below a side-by-side comparison of CPA with other treatments using data published in independent peer-reviewed medical journals. Please scroll down to your condition of interest to read the comparison data. To calculate your odds of pregnancy with Clear Passage® with more specialized information, please visit our “Calculate My Odds” pages.
Risk and Side Effects, and a Note About Surgery
Because the alternative of CPA is often surgery, the following risks and side effects apply to nearly all conditions comparing CPA to surgery:
Surgical risks:
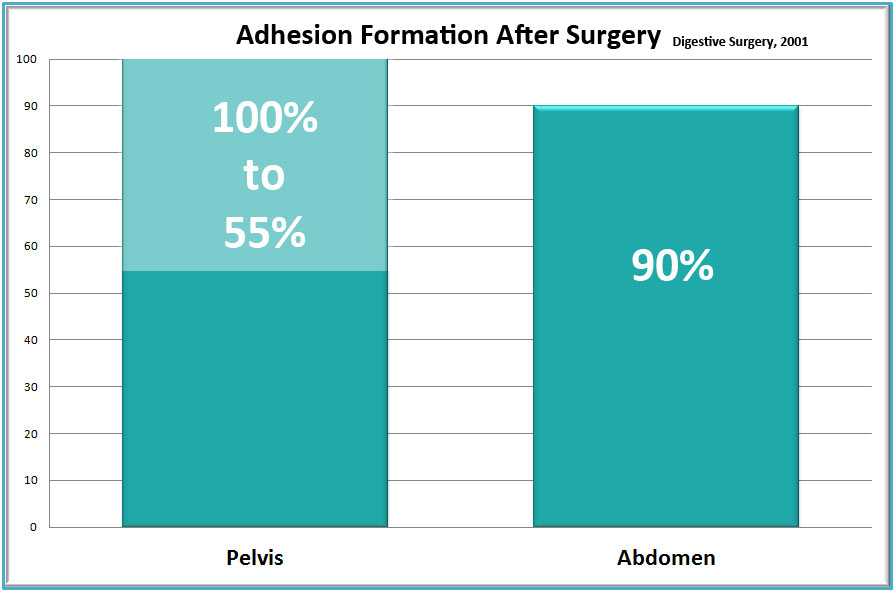
Post-surgical adhesions: Overwhelming evidence shows a primary (and nearly inevitable) risk of surgery is the formation of post-surgical internal scarring (adhesions). No matter how skilled the surgeon, the body creates glue-like adhesions after living tissues are cut or burned. Results of a 57-year review of the side effects of surgery (Liakakos et al., 2001) concluded:
“Adhesions occur in more than 90% of the patients after major abdominal surgery and in 55-100% of the women undergoing pelvic surgery. Small-bowel obstruction, infertility, chronic abdominal and pelvic pain, and difficult re-operative surgery are the most common consequences of abdominal and pelvic adhesions.”
Severe Infection is a major risk for bowel obstruction patients where the doctor is cutting through the intestines. Any leakage from the intestines into the body cavity where the patient was cut can cause an internal infection that can quickly become life-threatening. Per government statistics, 18% of all bowel resection patients are readmitted to the hospital within 30 days (HCUP Net, 2012). A related report in Lancet found that 35% of all open abdominal or pelvic surgery patients were readmitted to the hospital more than twice to treat post-surgical adhesions during the 10 years after their original surgery, with 22% of these ‘follow-up’ surgeries in the first year after surgery. The study noted that “readmissions continued steadily throughout the 10-year period” of the study (Ellis et al., 1999).
Inadvertent enterotomy: Adhesions can make surgery more difficult, obscuring vital structures behind sheets of scarred tissue. Unable to view clearly, a surgeon can inadvertently cut into a nearby organ, nerve or blood vessel. This is more of a concern in patients with extensive scarring (adhesions).
Surgical side effects:
Anesthesia: While most side effects from anesthesia are temporal (nausea, dry mouth, sore throat), data from several studies is being studied about possible brain damage from anesthesia. In an article from Scientific American (Storrs, 2014), the author notes that “Anesthesia may have lingering side effects on the brain, even years after an operation.”
Surgery:
- Short-term side effects: Side effects from surgery vary widely, but tend to include pain, swelling, soreness, loss of work and leisure time during recovery.
- Long-term and serious side effects: The primary lasting side effect of surgery is the formation of post-surgical adhesions [see graph]. Especially in the case of bowel obstruction surgery, there is concern for post-surgical infection, which can be life threatening, and/or require additional surgery.
Clear Passage® Approach (CPA):
CPA risks:
The primary documented risks with CPA are temporary soreness in the areas where we work.
CPA side effects:
CPA patients sometimes become fatigued during their treatment week; some undergo strong emotions as bound tissues are freed. These responses are generally temporary and dissipate within the week following therapy. CPA patients do not tend to lose work or leisure time, though we ask you to avoid heavy lifting and strenuous exercise for 7 to 10 days after therapy. Studies show that positive side effects of CPA included decreased pain and increased Function. Treatment that includes the female reproductive organs often show decreased intercourse pain, increased desire (libido), arousal, lubrication and orgasm. (Wurn et al., 2011; Wurn et al., 2004b)
Benefits and Success Rates: A Side-By-Side Comparison for Various Conditions
Benefits and success rates vary greatly per condition and procedure. We will present these by condition treated under each section below.
Female infertility:
Success rates treating female infertility using CPA and other procedures are very well documented. Published medical success rates are generally measured via pregnancy rates, so we used the same measure. In a large peer reviewed study of 1392 women housed in the U.S. National Library of Medicine (NLM), scientists compared the results of the CPA to published success rates for standard medical care. (Rice et al., 2015) These are the findings:
Blocked Fallopian Tubes: CPA success rates (in blue) compared well to studies of three different surgical techniques (in green) for pregnancies after opening blocked fallopian tubes. (Rice et al., 2015)
Most physicians advise that surgery to open blocked tubes is only appropriate to consider if the blockage is proximal (not near the uterus). Even in that case, most doctors note that a surgery to open a proximally blocked tube provides a woman with only a very brief window in which to conceive. In the largest study of its kind ever conducted, only 19% of tubes that were surgically opened remained open six months later. This does not appear to occur with CPA patients, many of whom have reported second and third children naturally with no further therapy.
It is important to note that the CPA success rate for opening blocked tubes was 69% for women who had never had surgery to their tubes, but only 35% for those who had undergone prior surgery to the fallopian tube – the lower number presumably due to post-surgical adhesions.
Polycystic ovarian syndrome (PCOS):
In a study of nearly 1400 women, CPA success rates (in blue) compared well to studies of surgery (middle bar) and medication (right bar) – both in green. (Rice et al., 2015)
Alternative treatment includes medication (22%), and either of two different surgeries:
- Ovarian wedging (cutting and removing a wedge out of the ovary), and
- Ovarian drilling (drilling holes in the ovary).
We encourage you to ask your physician about side effects of the medication s/he would prescribe. Surgical risks include creating additional adhesions from cutting and burning these delicate structures within the reproductive system. CPA results were much better in women who had not previously undergone surgery to the ovaries – presumably due to post-surgical adhesions that tend to attach like glue to the delicate reproductive structures, decreasing function.
Endometriosis infertility:
In a study of nearly 1400 women, success rates with CPA (blue bar at left) and endometriosis surgery (green bars center and right) are nearly identical, with a slight edge toward CPA, as shown here. (Rice et al., 2015)
Some studies indicate that post-surgical endometriosis pain and adhesion reformation is more prevalent at the sites of prior endometriosis surgery.
High FSH:
Women approaching the end of their reproductive years are often diagnosed with high FSH (follicle stimulating hormone) on day 2 – 5 of their cycle, as the ovary calls on the pituitary to create more and more FSH to help eggs mature. In a study of nearly 1400 women, 39% of women who are diagnosed infertile or subfertile due to high FSH became pregnant after using the CPA. (Rice et al., 2015)
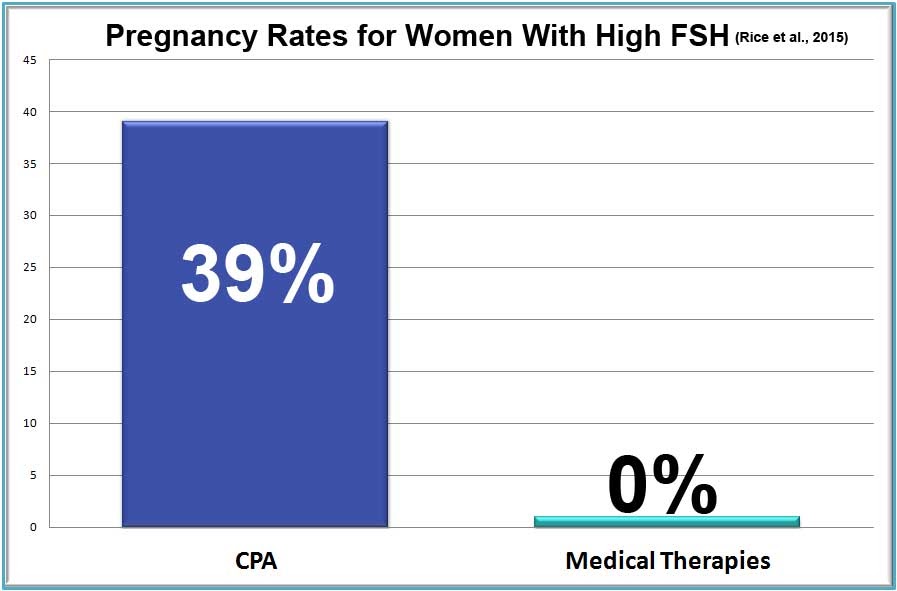
Medical treatments:
The only comparable medical technique requires an injection of FSH. Other than Clear Passage®️ no treatment for high FSH has been shown effective in medical studies.
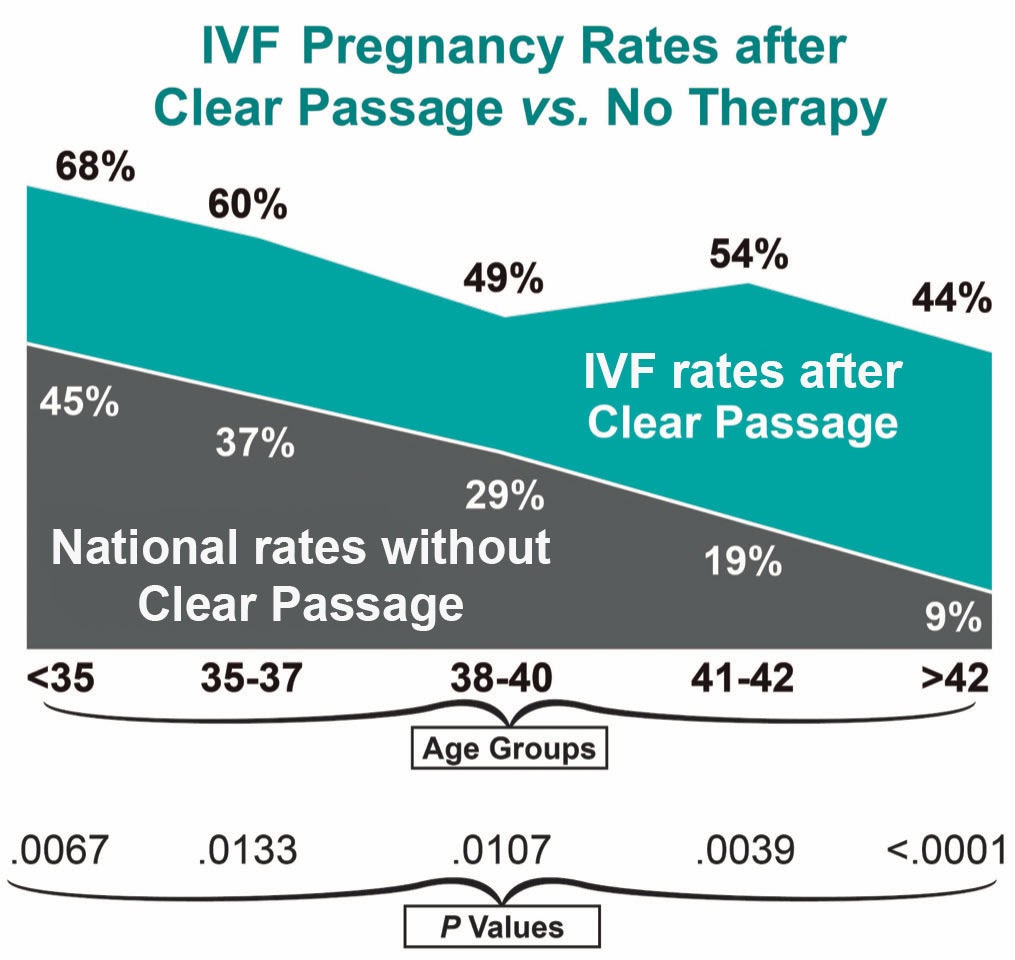
Pre-IVF therapy:
In a study of nearly 1400 women, overall post-transfer IVF pregnancy rates without CPA (37%) were compared to IVF pregnancy rates for women who had first undergone CPA therapy (56%). The overall rates are shown by age below, with pregnancy rates without CPA (in green), and with CPA, within 15 months before embryo transfer (in blue). (Rice et al., 2015) Rates with excellent statistical values are shown here for every age group, per CDC standards.
Small bowel obstruction
Measuring success treating small bowel obstruction (SBO) involves measuring a variety of concerns and symptoms. The primary concern for most patients is having another obstruction that requires hospitalization and surgery. Before therapy, our SBO patients often report symptoms that include pain, compromised diet, gastrointestinal problems. Generally, patients also report significant quality of life concerns, including fear of traveling away from their hospital, and concerns regarding social activities, such as visiting friends for meals or fear of attending a social event.
Two ways to measure success:
To measure our success addressing all of these symptoms and concerns:
- Eliminated Surgeries: We have very good data and excellent results eliminating future surgeries. With statistical results showing CP therapy decreased recurring total obstruction by 15 times the norm.
- Improved Quality of Life: Our scientists created and published a validated Quality of Life Questionnaire to measure symptoms and concerns. This document has now become an accepted part of U.S. medical literature for physicians and scientists to measure success with SBO patients. (Rice et al., 2014b)
In studies published to date, we are pleased to report that our patients have reported profound decreases in their required surgeries, and significant improvements in quality of life after therapy, in several areas.
Improved quality of life
Virtually all of these people live in fear of another obstruction that could happen at any time. Thus, we hired a biostatistician to design, validate and publish a questionnaire and rating tool to measure quality of life in the five major ‘domains’ where our patients were reporting concerns before therapy:
- Diet
- Pain
- Medication
- Quality of Life Issues, and
- Gastrointestinal (GI) Symptoms
The questionnaire was given to patients when they enrolled in the study, then again 90 days after the study closed. The biostatistician was able to measure changes (if any) between the start and end dates for both the Therapy and the Control Group.
Realizing that both the degree of pain and the ability to move freely affect Quality of Life, we added a “pain rating” section, and a section that compared ‘before and after’ Trunk Range of Motion for each participant.
- The Diet Domain assessed the diet of the subject from inability to tolerate any liquid to a normal solid food diet.
- The Pain Domain reported pain throughout the body, with oral intake of food or liquid, and with bowel function.
- The Gastrointestinal (GI) Symptom Domain quantified symptoms often associated with SBO such as nausea, emesis, bowel spasm and constipation.
- The Medication Domain reports the frequency of medications required to maintain bowel function.
- The Quality of Life Domain quantified the amount of time off work and social activities. In addition, it quantified each patient’s overall concern regarding their bowel function. We found that all of these tend to be major lifetime concerns for many people who experience recurring bowel obstructions.
RESULTS (direct quote from the study)
Despite histories of more prior hospitalizations, obstructions, surgeries, and years impacted by bowel issues, the 103 CP-treated subjects reported a significantly lower rate of repeat SBO than 136 untreated controls (total obstructions P = 0.0003; partial obstructions P = 0.0076).
Subjects treated with the therapy demonstrated significant improvements in five of six total domains in the validated Small Bowel Obstruction Questionnaire (SBO-Q).
Domains of diet, pain, gastrointestinal symptoms, quality of life (QOL) and pain severity when compared to post CPA treatment were significantly improved (P < 0.0001).
The medication domain was not changed in the CPA treated group (P = 0.176).
To talk to a therapist about how we can assist you in achieving your long-term goals, please visit our contact page or call us at (352)-336-1433.


