Overview
When diagnostic tests fail to show a cause of your pain, physicians who suspect a mechanical cause (e.g. adhesions, endometriosis) may suggest an exploratory surgery, hoping that the doctor can see and treat the cause of the pain or dysfunction.
Once medical and hormonal conditions have been ruled out, the pain or dysfunction is often thought to be mechanical in nature. If diagnostic images from X-ray, MRI, CT or ultrasound fail to show a cause, physicians tend to suspect that adhesions, internal scars that bind structures together, are causing the pain.
Treatment of adhesions that cause ‘unexplained pain’ can be conducted via surgery or a non‑surgical technique, the Clear Passage®️ Approach. Below, we compare and contrast these two approaches for treating unexplained pain with suspected adhesions.
Avoiding Surgery
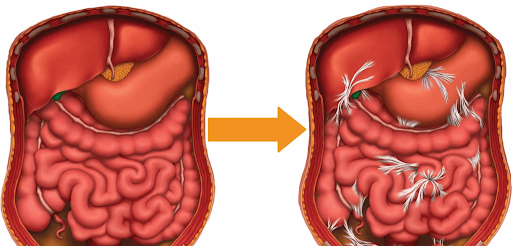
Adhesions in the abdomen or pelvis can become very serious, slowing or stopping the function of some of the body’s most important internal structures. Left untreated, they can cause or contribute to female infertility or end a person’s life by blocking the passage of food through the intestines. These adhesions generally lead to intense, debilitating pain by binding to strictures in the body with a pull that is exacerbated and provoked by inflammation. Surgery inevitably leads to more adhesions, making surgery a less than ideal treatment in many cases.
Overview of Treatment Options
According to medical literature, adhesions in the abdomen or pelvis can be addressed in two distinctly different ways:
- The Clear Passage®️ Approach
- Drugs and or Surgery
Clear Passage®️ Therapy to Decrease Adhesions
Description of the procedure. The Clear Passage®️ Approach is a manual physical therapy that uses no drugs or surgery. It has been cited in numerous studies and peer-reviewed medical journals for its ability to decrease adhesions. The studies show effectiveness with numerous types of pain and dysfunction caused by adhesions. “Before and after” studies by independent diagnostic physicians are included within some of the published studies.
The therapy is ‘all natural’ in that it is 100% ‘hands-on.’ Patients describe it as feeling like a very deep massage. At times, the therapy can sometimes be much lighter, depending on the area and depth being treated. Physical therapists use their hands to find adhered areas. Then, they work to deform and detach the tiny strands that comprise adhesions – similar to pulling out the strands of a nylon rope or pulling out the run in a sweater. They describe it as “pulling out salt-water taffy, in very slow motion.”
The therapy is site-specific for treating the adhered area. The therapists are experts at palpating and manipulating the soft tissues of the body – where adhesions often form. They use data from the patient’s history, direct feedback from the patient during therapy, and a thorough training and understanding of methods developed over 30 years to deform and detach the molecular/chemical bonds called cross-links that are at the core of adhesions. The usual protocol, cited in the studies, consists of 20 hours of therapy over the course of five days. You can view a short video of a Clear Passage®️ therapy session by clicking below.
Advantages of Therapy
No hospitalization. Therapy is performed in a private treatment room, one-on-one with a highly skilled therapist certified in the work. Patients are invited to bring a partner or family member along for company, if they like.
No anesthesia. The patient is awake and communicative during the procedure. Patient involvement is encouraged, with the patient invited to give feedback throughout the course of therapy.
Decreased risk. Risk is minimal. There is no cutting, no burning, no risk of side effects from anesthesia or medications, and no risk of inadvertently cutting through a nearby organ or other structure.
No foreign bodies are introduced. No staples, stitches, films or meshes are inserted into the body. No cameras, gas, lights or surgical instruments enter the body.
Side effects are mild,and transient. The most common side effects reported with therapy are temporary tenderness, aching, fatigue and hip or back pain. When they occur, these symptoms pass within a few days.
Improvements in other areas of the body. Because therapy focuses on detaching adhesions throughout the body, patients regularly report significant increases in flexibility and range of motion after therapy. Many report decreased pain and/or increased function in areas near the site where they are being treated. Some report this in areas where they had forgotten or had not realized they were having a problem, until therapy relieved the pain or tightness.
Written reports. After therapy, we send each patient a typed, detailed Initial Evaluation along with a typed Progress Report or Discharge Summary. If needed, we are glad to send you daily notes of every therapy session.
Disadvantages: Risks and Challenges of Therapy
Therapists cannot visualize the adhesions. Initially, we deduce the likelihood of adhesions by conducting a thorough review of your history and symptoms. To gain further insights, we may require diagnostic tests or documentation from your physician. During therapy, we palpate the areas of your body related to your symptoms and other areas where we note spasm, tightness or increased temperature. Because our therapists are skilled professionals who have been practicing manual therapy for most of their professional lives, they are experts at palpating the body.
Costs of therapy are generally a fraction of the cost of surgery; as with surgery; insurance reimbursement may vary based upon your insurer and your plan. Clear Passage®️ is an out-of-network provider for your insurer.
Travel and time are a consideration. Therapy generally takes five days (e.g., Monday – Friday); it is only provided by trained, certified therapists in several cities in the U.S. and U.K. The 5-day program is designed for out-of-town and out-of-country patients. Most patients fly in on the weekend, start therapy Monday morning and are done Friday afternoon.
Surgery to Decrease Abdominopelvic Adhesions
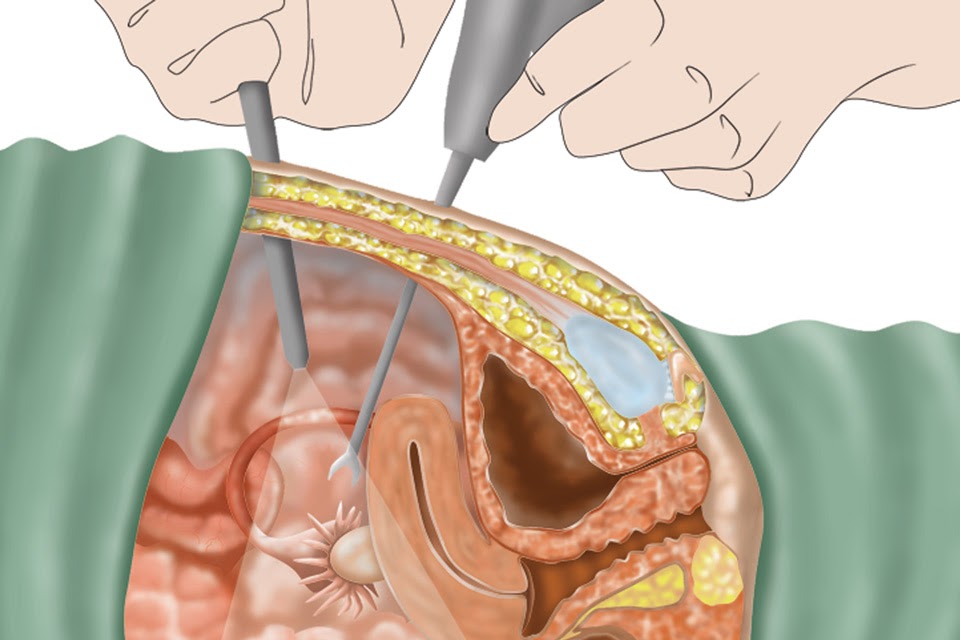
Description of common procedures. The intent of adhesiolysis surgery is to cut or burn adhesions to help return the body to an earlier state of mobility and function. In a laparoscopy, the physician puts the patient under general anesthesia, then cuts several openings (ports) in the body. These ports serve several functions. One is used to fill the cavity with a gas to help separate the organs so the surgeon can create a space in which to insert surgical instruments to access the adhesions. Using the other ports, the doctor will insert a light, generally a camera, and the surgical instrument(s) with which they can cut or burn adhesions that they see. You can observe a laparoscopy to decrease adhesions by clicking here.
When adhesions are extensive, the physician may elect to perform an open surgery called a laparotomy. In that surgery, the body is cut open with a scalpel and the sides may be separated with a metal retractor. Next, the physician enters with a scalpel, laser or other surgical instrument to cut or burn any adhesions s/he may find. S/he will repair or cauterize any bleeding that occurs, and may check the area for other problems before exiting the body, stitching and/or stapling it shut, and sending the patient to a room where staff can monitor the patient’s recovery.
Advantages of Surgery
Direct visualization. The surgeon’s ability to directly see, then cut or burn adhesions is a major advantage.
Observe nearby areas. In addition to treating the adhered area, the physician can visualize nearby structures and assess their health and condition, noting any additional areas that may be of concern.
Operative report. The doctor will dictate a report that describes what s/he observes and the procedures s/he performed during the surgery.
Pre-Treatment Screening (Surgery and Therapy)
Both therapy and surgery require patients to be screened for appropriateness and contraindications before treatment.
Screening before therapy. Before therapy, Clear Passage®️ directors consult applicants to review goals, risks and potential benefits they can expect. We conduct a thorough review of the applicant’s history of healing events (prior surgery, trauma, infection, endometriosis, etc.) to determine if and where adhesions have likely formed, and the problems they may be causing.
We screen applicants for two reasons:
- To determine the likelihood that we can help an applicant reach his/her goal,
- To rule out contraindications that could decrease effectiveness of therapy or cause problems.
Screening before surgery. Before surgery, physicians consult patients to review the goals, risks and potential benefits they can expect from the procedure. They may order diagnostic tests to help rule out contraindications, such as active infection, and to help identify problem areas in the body that should be assessed during surgery. It is reasonable to ask your doctor about the likelihood of new adhesion formation after surgery.
Disadvantages: Surgical Risks and Challenges
Anesthesia complications. Recent studies note concerns about mild to moderate brain damage for patients who undergo one or more sessions of general anesthesia. (Perousanksy & Hemmings, 2009)
Inadvertent enterotomy. When a patient has significant adhesions, it can be difficult for the doctor to see the structures beneath them. Thus, a surgeon can unintentionally cut into a nearby healthy organ or other structure – called an inadvertent enterotomy (IE). An IE can cause serious problems or death. In a study from the Journal of the Society of Laparoscopic Surgeons, authors note that:
- “IE in laparoscopic abdominal surgery is underreported.”
- “Death from IE is not uncommon.”
- “IE was the most common laparoscopic complication at our hospital.” (Binenbaum & Goldfarb, 2006)
Hospitalization during recovery. Most patients must undergo a hospital stay after any abdominal or pelvic surgery. Patients are monitored to ensure their recovery and that there are no immediate post-surgical complications or infections.
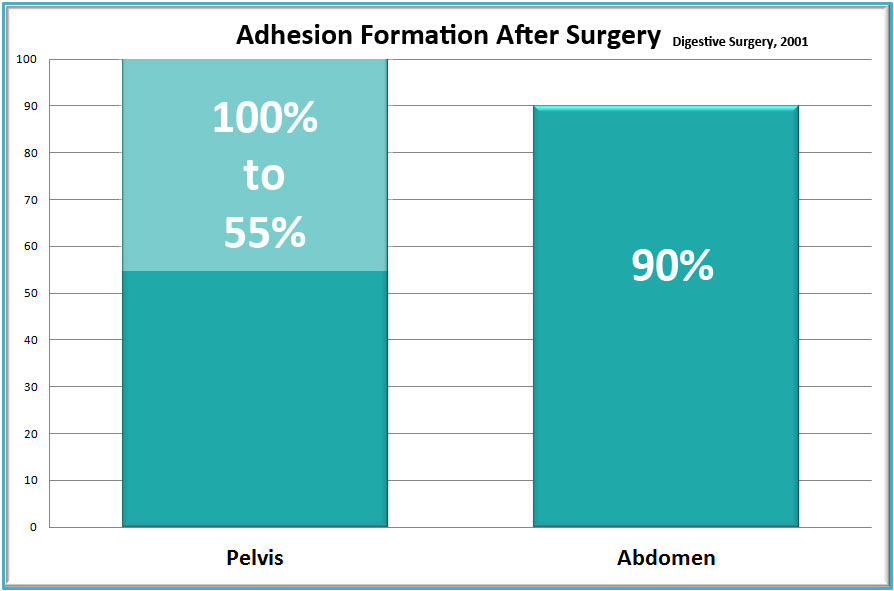
New adhesions generally form after surgery. Data compiled from over 50 years of abdominal and pelvic surgeries shows that nearly all surgeries cause new adhesions to form. Thus, despite the skills of the finest surgeon, adhesions often recur, sometimes worse than before the surgery to remove them. Because surgeries cause adhesions, some or our patients feel stuck in an unending cycle of adhesions-surgery-pain-adhesions-pain-adhesions.
Pre-Treatment Screening (Surgery and Therapy)
Both therapy and surgery require patients to be screened for appropriateness and contraindications before treatment.
Screening before therapy. Before therapy, Clear Passage®️ directors consult applicants to review goals, risks and potential benefits they can expect. We conduct a thorough review of the applicant’s history of healing events (prior surgery, trauma, infection, endometriosis, etc.) to determine if and where adhesions have likely formed, and the problems they may be causing.
We screen applicants for two reasons:
- To determine the likelihood that we can help an applicant reach his/her goal,
- To rule out contraindications that could decrease effectiveness of therapy or cause problems.
Screening before surgery. Before surgery, physicians consult patients to review the goals, risks and potential benefits they can expect from the procedure. They may order diagnostic tests to help rule out contraindications, such as active infection, and to help identify problem areas in the body that should be assessed during surgery. It is reasonable to ask your doctor about the likelihood of new adhesion formation after surgery.
Related Content:
Avoid Surgeries: Adhesions | Blocked Fallopian Tubes | Endometriosis | PCOS | SBO | Surgery Risks | Tailbone