Overview
Fallopian tubes are the delicate environment where life begins. Each of these two narrow structures is the place where a one-celled egg can meet a sperm, creating a life that will continue its journey to implantation in the uterus. As such, this tiny organ must be patent (open) and able to function freely and without restriction for a pregnancy to occur.
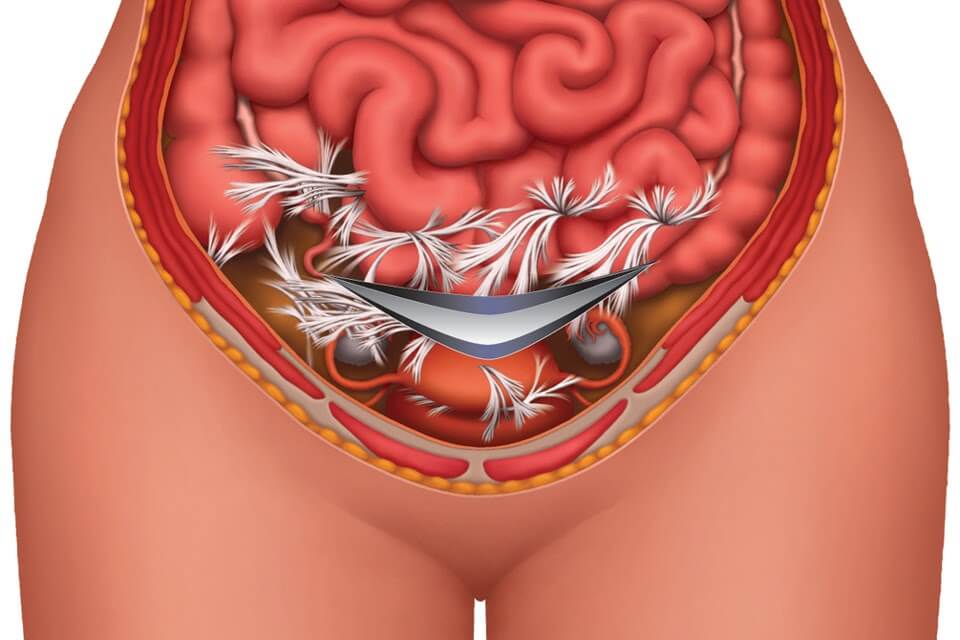
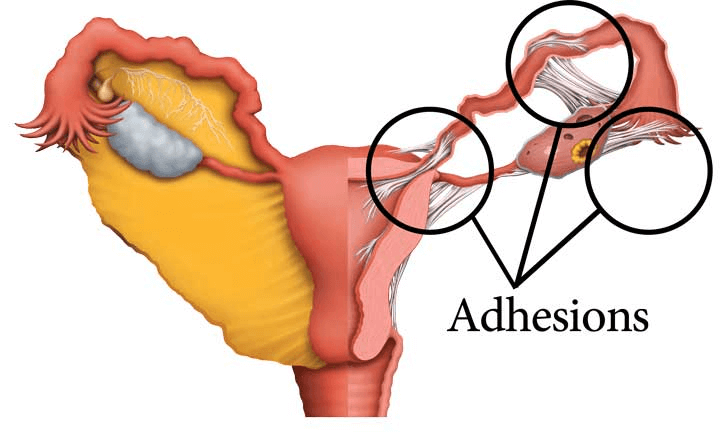
The primary cause of tubal occlusion (blockage) is internal scarring by adhesions. Adhesions form as glue-like bonds in the reproductive tract as the body’s initial response to pelvic inflammatory disease (PID), endometriosis, sexually transmitted infection, a prior surgery or ectopic pregnancy.
After adhesions form, they can remain in the body for a lifetime. When they form at the distal end of the tube (near the ovary), they can cause swelling of the tube in a condition called hydrosalpinx. Adhesions can form and spread into any part of the tube, and anywhere in the pelvis. Wherever they form, they can squeeze reproductive structures or attach them to other structures, further decreasing fertility.
| PROCEDURE | PREGNANCY RATE | COSTS |
| Clear Passage® Bodywork | 39.33% ii | $6,500 |
| In Vitro fertilization (IVF) | 30.87% iii | $15,000 – $30,000 iv |
| IVF after Clear Passage | 56.16% ii, iii | $21,500 – $36,500 iv |
Avoiding Surgery
Click here to view a surgery to open blocked fallopian tubes
The interior dimension of a fallopian tube is tiny, designed to transport a single celled egg to meet much tinier sperm, in order to create a pregnancy. The inner lining of a fallopian tube looks like a lush underwater garden, lined with microscopic cilia that help the process along. The act of cutting into such delicate structures to perform a surgical repair is both challenging and problematic. While surgery can sometimes open a blocked fallopian tube, physicians know that there is significant risk of post-surgical adhesions – scar tissue that tends to re-block the tube within a few months.
Surgery to clear proximal occlusion (blockage near the uterus)
Surgery is considered when the site of the blockage is proximal — near the uterus. In this instance, the physician can often access the occlusion by inserting a sterilized wire, sometimes with a tiny balloon attached into the tube via the uterus. Thus, the doctor can avoid the costs and risks of the additional post-surgical adhesions associated with laparoscopy. Risks with this minimally invasive technique include pinpoint perforations of the vagina, cervix, uterus or fallopian tube as the wire passes through these structures.
Surgery to clear distal occlusion and hydrosalpinx (blockage in the mid or distal tube)
Most physicians will not operate on tubes that are blocked beyond the portion closest to the uterus. Designed to carry individual cells, the tube is so tiny and delicate that post-surgical scars tend to re-block the tube, even after a successful surgery. For this reason, surgeons generally avoid any attempt to open tubes that are blocked beyond the uterine opening. In some cases such as hydrosalpinx (swollen tube) the physician will recommend removal of the blocked tube, and referral for in vitro fertilization (IVF).
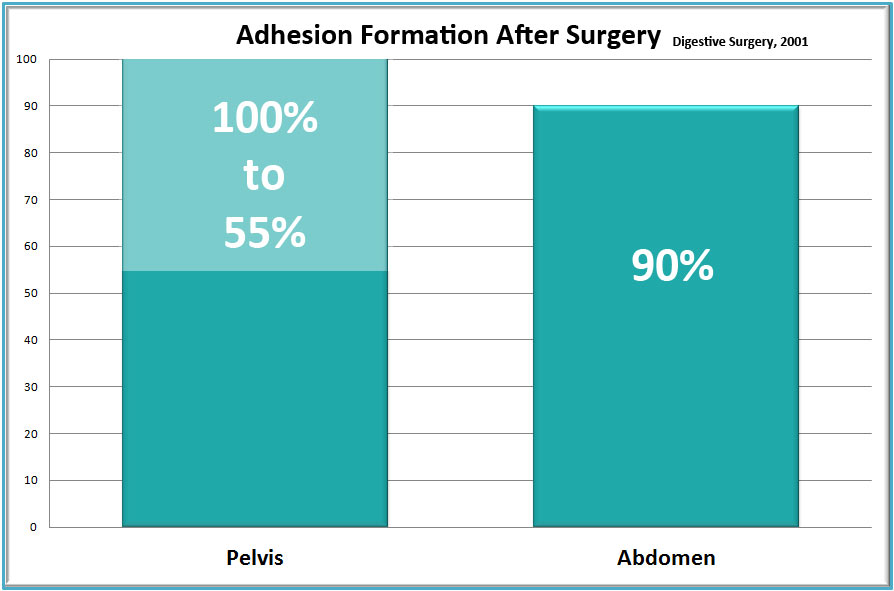
In a mammoth 58-year study of medical literature, researchers found that adhesions occur in more than 90% of patients following major abdominal surgery and in 55-100% of women undergoing pelvic surgery. The study noted that “small-bowel obstruction, infertility, chronic abdominal and pelvic pain, and difficult re-operative surgery were the most common consequences of the adhesions.” Underlining the ongoing difficulty adhesions can cause, the study concluded “Despite elaborate efforts to develop effective strategies to reduce or prevent adhesions, their formation remains a frequent occurrence after abdominal surgery.” In short, post-surgical adhesions are a major problem for physicians and patients alike.
With over a dozen citations and studies published in medical journals, we can quantify success rates for the dozens of women whose tubes we have opened – most of whom are now mothers. To date, Clear Passage® has seen over 1,000 babies born to our patients – women diagnosed infertile before they came to us for therapy.
Overview of Treatment Options
Clear Passage®️ Therapy to Open Tubes, Improve Function and Fertility
Over the last 20 years, numerous peer-reviewed studies and citations have cited Clear Passage® therapy for our ability to increase fertility by decreasing adhesions. Several of the studies have centered on its abilities to help women with occluded fallopian tubes, without the need for surgery.
Description of the procedure. The Clear Passage® approach is a manual physical therapy; it is ‘all natural’ in that it is 100% percent ‘hands-on.’ While some patients describe CP as feeling like a very deep, site-specific, massage others note that it can sometimes be much lighter, depending on the area and depth being treated. Highly trained and certified in this therapy, our licensed therapists use their hands to deform and detach the tiny strands that comprise adhesions – similar to pulling out the strands of a nylon rope or pulling out the run in a sweater. Therapists sometimes say it “feels like I’m pulling out taffy, in very slow motion.”
The therapy is very site-specific for adhesions. Therapists certified to perform this work are experts at palpating and manipulating the soft tissues of the body – where adhesions generally cause problems with infertility. They use data from the patient’s history along with direct feedback from each patient during therapy. Each provider receives extensive training to understand the methods developed by our directors over 30 years to deform and detach the molecular/chemical bonds to the delicate cilia on the inner walls of the fallopian tube or bind the tube to nearby structures. When we are successful releasing those bonds, the tubes tend to return to an earlier state of pain-free mobility and function.
The usual protocol cited in the published studies, consists of 20 hours of therapy spaced over five or more days. Patients often start therapy Monday morning, receive four hours of therapy a day with a break for lunch, and are done Friday afternoon. Other than that, they are free to work, rest or take a break from a busy lifestyle. Many women set aside these five days as a “special time to help their bodies heal.” Learn more and view a short video of Clear Passage®️ treatment for blocked tubes.
Advantages of Therapy
No hospitalization. Therapy is performed in a clean, private treatment room, one-on-one with a highly skilled physical therapist certified in the work. You are invited to bring a partner or family member along for company, if you like.
No anesthesia. While risks of anesthesia are small, they do exist. Our patients are awake and communicative during the procedure. We actively encourage patient involvement and feedback. In doing so, we invite each patient to be an active member of the team that is working hard to achieve her results. In addition, we provide education in the formation and deformation of adhesions anywhere in the body. We teach each patient self-treatment techniques she can use for her entire life. This education and communication is not available to a person under anesthesia.
Decreased risk. Risk is minimal because there is no cutting or burning. There is no risk of forming post-surgical adhesions that can re-bind the delicate reproductive structures or spread to other organs. Therapy also avoids the surgical risk of inadvertently cutting through a nearby structure, such as the bowel, bladder or even stomach (we have seen all of these).
No foreign objects are placed deep within your body. No stitches, staples, films or meshes are inserted into the body. No cameras, gas, lights, surgical instruments or contaminants enter the abdominal cavity from the ‘outside world.’
Side effects are mild, transient – or positive. The most common side effects patients report are temporary tenderness, aching, fatigue and hip or back pain. When they occur, these symptoms are minimized with an anti-inflammatory or a 20 minute compress or soak with epsom salts, in the evening after therapy. Other side effects cited in medical literature are positive. These include decreased intercourse pain, increased desire, arousal, lubrication and orgasm (including first-time orgasms).
Verified success rates. Several peer-reviewed studies measure the ability of this therapy to decrease pain if any and increase fertility for women diagnosed with blocked fallopian tubes. In a ten-year study with hundreds of participants, our fertility success rates for women with blocked tubes rivaled or surpassed those of surgery. You may view all of our success rates by clicking here.
Improvements in other areas of the body. Because therapy focuses on detaching adhesions throughout the body, it is common for patients to report significant increased flexibility and range of motion after therapy. In addition, many report decreased pain and/or increased function in areas near the sites where they are being treated. Some report this phenomenon in areas they had forgotten or had not realized they were having a problem with, until therapy relieved the pain or tightness.
Written reports. After therapy, we send each patient a typed, detailed Initial Evaluation along with a typed Progress Report or Discharge Summary. If needed, we are glad to send you daily notes of every therapy session.
Risks and Challenges of Therapy
Therapists cannot visualize the adhesions. Initially, we deduce the likelihood of adhesions by conducting a thorough review of your history and symptoms. To gain further insights, we may request diagnostic tests or documentation from your physician. As well as treating the tubes and uterus, we palpate any areas where we note spasm, asymmetry, thickened tissues or increased temperature. Because our therapists have been doing manual therapy for most of their professional lives, they are experts at palpating the body.
Costs of therapy are generally a fraction of the cost of surgery; as with surgery, insurance reimbursement may vary based upon your insurer and your plan. Clear Passage®️ is an out-of-network provider for your insurer.
Travel and time are a consideration. Designed for local and out-of-town patients, therapy is given for 20 hours over a five-day period (e.g., Monday – Friday). It is provided by trained, certified therapists in several cities in the U.S. and U.K.
No medical techniques have 100% success rate. If we are unable to open your tubes, your chances for a successful IVF performed within 15 months after therapy increase by roughly 50%, per published studies. View our success rates.
Surgery or Drugs to Open Fallopian Tubes
No pharmaceutical, tampon, lotion or ingestible has ever been shown to open blocked fallopian tubes.
Description of surgery. The intent of tubal surgery is to cut or burn the adhesions blocking the tube, then reattach any options that were cut or seperated. In a laparoscopy, the physician puts the patient under general anesthesia, then cuts several holes (ports) in the body. One of the ports is used to fill the cavity with a gas to separate the organs so that the surgeon can create a path through which s/he can visualize the structures s/he needs to remove or repair. Using the other ports, the doctor will insert a light, camera, and surgical instrument(s) with which they can cut or burn the tube to eliminate any blockage. Click here to view a surgery to open blocked fallopian tubes
When adhesions are extensive, the physician may elect to perform an open surgery called a laparotomy. In that surgery, the physician cuts the body open via a longer incision and then may separate the sides with a metal retractor. Next, the surgeon enters with a scalpel, laser or other surgical instrument to repair the tubes, and to cut or burn any adhesions s/he may find. S/he will repair or cauterize any bleeding that occurs and will often check for other problems before exiting the body and sending the patient to a room for post-surgical recovery.
Advantages of Surgery
Direct visualization. The surgeon can directly see the area and visually assess the internal condition. In some cases, s/he may not be able to see through thick blankets of adhesions. This can lead to problems (inadvertent enterotomy) noted below.
Observe nearby areas. In addition to attempting to repair the tube, the physician can see and assess the condition of nearby structures, noting any areas that may be of concern.
Operative report. As with therapy, the doctor will dictate a report that describes what s/he observes and the procedures s/he performs during the procedure.
Surgical Risks and Challenges
Anesthesia complications. Recent studies have raised possible concerns about neurotoxicity, with mild to moderate brain damage for patients who undergo one or more sessions of general anesthesia.
Inadvertent enterotomy. When a patient has significant adhesions, it can be difficult for the doctor to see the structures beneath them. Thus, a surgeon can unintentionally cut into a nearby healthy organ or other structure – called an inadvertent enterotomy (IE). An IE can cause serious problems or death. Authors from a study in the Journal of the Society of Laparoscopic Surgeons note:
- “Death from IE is not uncommon”
- “IE in laparoscopic abdominal surgery is underreported”
- “IE was the most common laparoscopic complication at our hospital”
Hospitalization during recovery. Some surgeries are followed by a hospital stay, during which patient recovery can be monitored for post-surgical complications or infections.
New adhesions generally form after surgery. It is a well-accepted medical fact that nearly all surgeries in the abdomen or pelvis cause new adhesions to form. Thus, pain and adhesions can recur – sometimes worse than before the surgery to remove them.
Risks of laparoscopy include:
- Hernia,
- Infection,
- Blood clots,
- Adverse reactions to anesthesia,
- Abdominal inflammation or infection,
- Bleeding and the potential need for a blood transfusion,
- Inadvertent enterotomy (mistaken damage to internal structures, e.g., blood vessels, stomach, bowel, bladder, ureter.)
Specific conditions that can increase your risk of complications during surgery include:
- Stroke
- Obesity
- Diabetes
- Smoking
- Seizures
- Drug allergies
- High blood pressure
- Obstructive sleep apnea
- History of heavy alcohol use
- History of adverse reactions to anesthesia
- Medications, such as aspirin, that can increase bleeding
- Other medical conditions involving your heart, lungs or kidneys
Pre-Treatment Screening (Surgery and Therapy)
Screening every patient for appropriateness and contraindications before therapy or surgery is a necessary part of pre-treatment workup.
Screening before therapy. Clear Passage®️ directors and staff consult applicants to review goals, risks and potential benefits that they can expect from therapy. We conduct a thorough review of your history of healing events (prior surgery, trauma, infection, endometriosis, etc.) to determine if and where adhesions have likely formed and how they might be causing problems. In addition, we may require additional tests or correspondence from your physician before we can accept you for therapy.
Screening before surgery. Your surgeon should consult with you to review the goals, risks and potential rewards you can expect from the procedure. They may order diagnostic tests to help rule out contraindications, such as active infection, and to help identify problem areas in the body for that should be assessed during surgery.
Liakakos, T., Thomakos, N., Fine, P., Dervenis, C., & Young, R. (2001). Peritoneal adhesions: etiology, pathophysiology, and clinical significance. Recent advances in prevention and management. Dig Surg, 18(4), 206–273
Perousanksy, M. and Hemmings Jr, H.C. (2009). Neurotoxicity of General Anesthetics: Cause for Concern? Anesthesiology, 111(6), 1365-1371. Binenbaum, S. & Goldfarb, M. (2006). Inadvertent enterotomy in minimally invasive abdominal surgery. Journal of the Society of Laparoendoscopic Surgeons, 10(3): 336-340
Related Content:
Avoid Surgeries: Adhesions | Blocked Fallopian Tubes | Endometriosis | PCOS | SBO | Surgery Risks | Tailbone