Overview
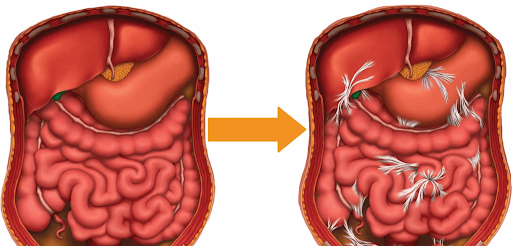
Small bowel obstruction creates major challenges for physicians and their patients. While a total small bowel obstruction is life-threatening and must often be dealt with surgically, it is accepted fact that surgery is the number one cause of recurring bowel obstructions. Thus, the last resort medical treatment for small bowel obstruction is also the primary cause of future obstructions, underlining the need for a non-surgical treatment that can break this vicious cycle.
Many people who have undergone surgery or infection in the abdomen undergo recurring “partial small bowel obstructions” due to internal adhesions squeezing or kinking the intestines. In these cases, food may finally pass, often aided by a hospital visit. The hospitalization generally includes the insertion of a naso-gastric (NG) tube through the nose into the stomach. Hospital staff will turn on an electric pump designed to constantly empty the stomach contents and relieve pressure on the digestive tract. The physician will often insert intravenous lines to introduce fluids for hydration, or narcotic pain relief, in an attempt to relax and hydrate the bowel, so that food will pass. Similar intravenous lines will provide nutrition since the bowels no longer work. Patients describe the experience as a scary, uncomfortable, and harrowing experience that can take many hours or days to clear.
Published Success Treating Bowel Obstruction
| 90%[fn] | 67%[fn] | 35%[fn] | 67%[fn] | 83%[fn] |
| Preventing Surgery | Pain Reduction | Improved Diet | Improved Quality of Life | Decreased Medications |
Avoiding Surgery
After a partial bowel obstruction, the patient’s ongoing concern is that despite the obstruction clearing, nothing has structurally changed. The patient is sent home with the advice “This may and probably will happen again.” Thus, many patients feel as if they are living with a time bomb in their gut, concerned with what they can eat, what social or work activities they can and cannot do, whether they can travel, etc. By far, their greatest fear is “What happens next time – if the obstruction does not clear?”
Treating the adhesions that cause recurring bowel obstructions without surgery is considered a major advance. Our manual (hands-on) physical therapy has been shown to greatly improve quality of life and significantly decrease the incidence of small bowel obstruction in patients who receive the therapy. To date, we know of no other non-surgical treatment actually shown to clear adhesions that obstruct the bowel.
Break free from the cycle of recurrent small bowel obstructions and regain control of your life with Clear Passage Physical Therapy’s Free Consult and Request Info – discover their groundbreaking, non-surgical approach that has been clinically proven to reduce adhesions, decrease pain, and significantly improve quality of life for patients suffering from this debilitating condition. To learn more, visit our Apply to Therapy page.
Treatment Options For Recurrent Bowel Obstructions
Clear Passage®️ Therapy to Decrease Adhesions
Description of the procedure. The Clear Passage® approach is a manual physical therapy that uses no drugs and no surgery. It has been cited in peer-reviewed medical texts and journals for its ability to decrease adhesions in the abdomen and pelvis, non-surgically. Some of the published studies include ‘before and after’ images and reports of individual patients prepared by independent diagnostic physicians. Others examine the effects of the therapy on treating adhesions for conditions, including recurring small bowel obstruction. Some studies show that results of the therapy equal or exceed the results of surgery, for improving structure and function.
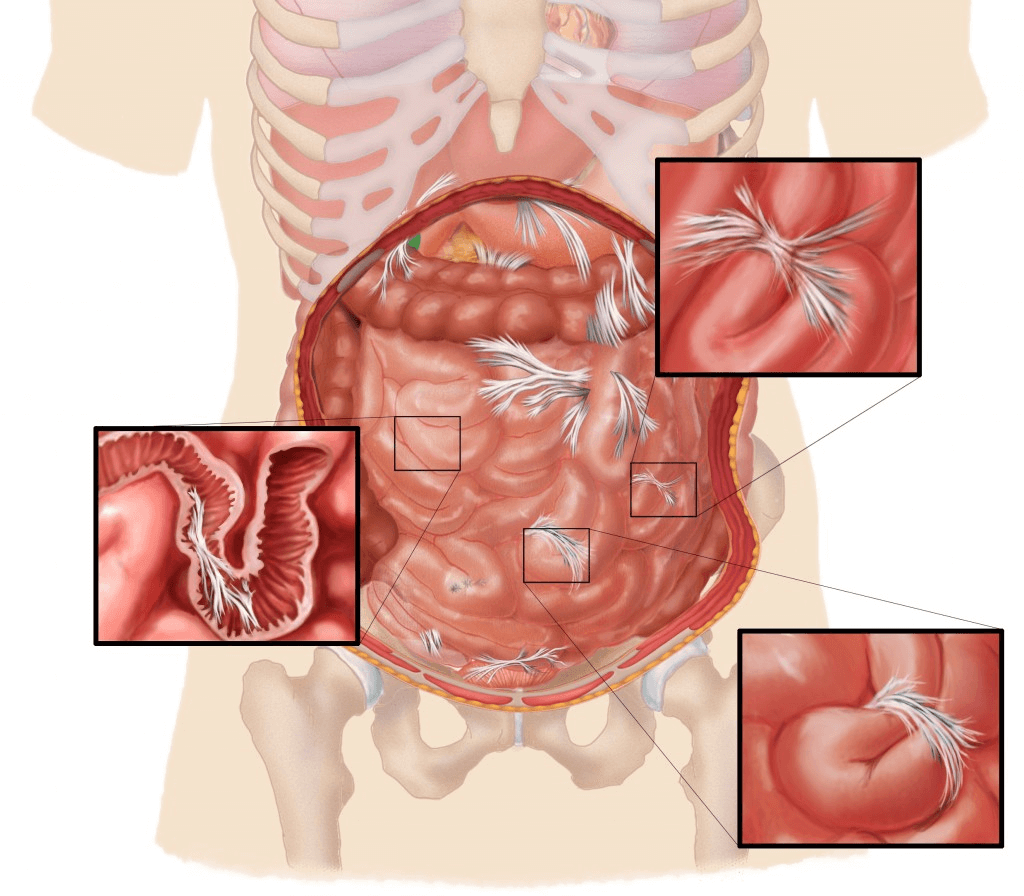
The therapy is ‘all natural’ in that it is 100 percent ‘hands-on.’ Many patients describe it as feeling like a very deep massage. Our physical therapists use their hands to locate adhered areas of the body related to the patient’s pain or symptoms. They then transition to very site-specific techniques to deform and detach the tiny strands that comprise adhesions. Therapy may be compared to pulling out the strands of a nylon rope or pulling out the run in a sweater. Our therapists describe it as feeling like “pulling out salt-water taffy, in very slow motion.”
Our therapists are experts at palpating and manipulating the abdomen and pelvis, where bowel adhesions cause problems. They use data from each patient’s history and direct feedback from the patient during therapy, along with training and understanding of methods developed over 30 years to locate and detach adhesions. The protocol cited in the studies consists of 20 hours of therapy, spaced over five or more days. View a short video of what Clear Passage®️ therapy is like.
Advantages of Therapy
No hospitalization. Therapy is always performed in a private treatment room, one-on-one with a highly skilled therapist certified in the work. Patients may bring a partner or family member along for company, if they like.
No anesthesia. Without general anesthesia, there is no risk of neurotoxicity to the brain or other areas of the body. The patient is not only awake and communicative during the procedure, we encourage patient involvement; each patient is invited to give feedback throughout the course of therapy. We feel that involving each patient in her/his care and soliciting their feedback during each therapy session generates better results.
Decreased risk. Risk is minimal. There is no cutting or burning, no risk from anesthesia, and no risk of inadvertently cutting through a nearby organ or other structure.
No foreign bodies are introduced. No staples, stitches, films or meshes are inserted into the body. No cameras, gas, lights or surgical instruments enter the body.
Side effects are mild and transient. The most common side effects reported with therapy are temporary tenderness, aching, fatigue and hip or back pain. Temporary soreness is generally relieved with a 20 minute epsom salt bath or compress in the evening.
Improvements in other areas of the body. Because therapy focuses on detaching strong adhesions that tend to form in various areas of the body, most patients report increases in flexibility and range of motion after therapy. Many report decreased pain and/or increased function in areas near the site where they are being treated – or even at distal sites. This pain reduction is often noted in the low back due to the freeing of abdominal adhesions from the front of the lumbar vertebrae. Some patients report improvements in areas where they had forgotten or had not realized they were having a problem, until therapy relieved the pain or tightness.
Written reports. After therapy, we send each patient a typed, detailed Initial Evaluation along with a typed Progress Report or Discharge Summary. If needed, we are glad to send you daily notes of every therapy session.
Disadvantages: Risks and Challenges of Therapy
Therapists cannot visualize the adhesions. Initially, we deduce the likelihood of adhesions by conducting a thorough review of each patient’s history and symptoms. To gain further insights, we may require diagnostic tests or documentation from your physician. During therapy, we palpate the areas of your body related to your symptoms and other areas where we note scarring, tightness, spasm or increased temperature. Because our therapists have been practicing manual therapy for most of all their entire professional life, they are experts at palpating and treating the body.
Costs of therapy are generally a fraction of the cost of surgery. As with surgery, insurance reimbursement may vary based upon your insurer and your plan. Clear Passage®️ is an out-of-network provider for your insurer. When considering the costs, we encourage patients to measure the cost of their quality of life and peace of mind vs. the sacrifices you make due to living with adhesions. Download our Insurance PDF to send to your insurance.
Travel and time are a consideration. Therapy generally takes five days (e.g., Monday – Friday); it is only provided by trained, certified therapists in several cities in the U.S. and U.K. The 5-day program is designed for out-of-town and out-of-country patients. We suggest that patients with a history of bowel obstructions remain in town for an extra day before returning home. The goal is to allow the body to return to homeostasis before undergoing changes in bowel air pressure that can accompany airline flight.
Surgery to Decrease Abdominopelvic Adhesions
Description of common procedures. Some patients with recurring bowel obstructions are encouraged to undergo a surgery to decrease adhesions in the abdomen or pelvic. The intent of adhesion surgery (adhesiolysis) is to cut or burn adhesions affecting the bowel and return the intestines to an earlier state of mobility and function. In a laparoscopy, the physician places the patient under general anesthesia and then cuts several holes (ports) in the body. Using one of these ports, the doctor will first fill the abdominal cavity with gas to separate the organs. This separation allows the surgeon to view a path to insert the surgical instruments s/he will use to cut or burn adhesions affecting the bowel. The doctor will also insert a light and a camera through the other port(s). You can observe a laparoscopy to decrease adhesions by clicking here.
When intestinal adhesions are extensive, the physician may perform or transition to an open surgery called a laparotomy. In that surgery, the body is cut open with a scalpel, then the skin and outer layers are separated with a metal retractor. Next, the physician enters with a scalpel, laser or other surgical instrument to cut or burn any adhesions s/he may find that are affecting the intestines. S/he will repair or cauterize any bleeding that occurs, and may check the area for other problems before exiting the body. Finally, s/he will close the body with stitches, and send the patient to a room where recovery can be monitored. You can view an open bowel resection by clicking here.
Advantages of Surgery
Direct visualization. The surgeon can directly see, then burn or cut adhesions that do not appear on diagnostic tests such as MRI or CT scan. Complications can occur in patients with significant adhesions if the doctor has difficulty seeing through the layers s/he is cutting (see below).
Observe nearby areas. In addition to treating the adhered area, the physician can visualize nearby structures. Thus, s/he can note and possibly treat any other problem areas in the vicinity.
Operative report. The doctor will dictate a report that describes what s/he observes and the procedures performed during the surgery.
Disadvantages: Surgical Risks and Challenges
Anesthesia complications. Recent studies have considered whether general anesthesia may have a neurotoxic effect on the brain or other areas of the body. (Perousanksy & Hemmings, 2009)
Inadvertent enterotomy. When a patient has significant adhesions, it can be difficult for the doctor to see the structures beneath them. Thus, a surgeon can unintentionally cut into a nearby healthy organ or other structure – called an inadvertent enterotomy (IE). An IE can cause serious problems or death. In a study from the Journal of the Society of Laparoscopic Surgeons, authors note that:
- “IE in laparoscopic abdominal surgery is underreported.”
- “Death from IE is not uncommon.”
- “IE was the most common laparoscopic complication at our hospital.” (Binenbaum & Goldfarb, 2006)
Hospitalization during recovery. Abdominopelvic lysis of adhesions is a major surgery, and most patients undergo a hospital stay afterwards. During this time, the patient’s condition closely monitored to ensure recovery and avoid post-surgical complications or infections.
New adhesions generally form after surgery. A mammoth 50-year review of abdominal and pelvic surgery in the U.S. revealed that nearly all abdominal and pelvic surgeries cause new adhesions to form. Thus, adhesions can recur – sometimes worse than before the surgery to remove them.
Pre-Treatment Screening (Surgery and Therapy)
Both therapy and surgery require patients to be screened for appropriateness and contraindications before treatment.
Screening before therapy. Before we can accept you for therapy, our staff will conduct a thorough review of your history of healing events (prior surgery, trauma, infection, endometriosis, etc.) to determine where adhesions have likely formed and how they might be causing problems related to your symptoms and complaints. We then consult with each patient to review goals, risks and the potential benefits they can expect.
We want you to do well and to have a reasonable chance to reach your goals. We will accept you if we feel we can help you; we will alert you if we have concerns that you will not do well with therapy. Similarly, we will not accept you if we feel that you will not have a favorable outcome.
Screening before surgery. Before surgery, your physician may order diagnostic tests to help rule out contraindications, such as active infection, and to help identify problem areas in the body that should be assessed during surgery. Your doctor should consult you to review the goals of surgery, along with the risks and potential rewards you can expect. We encourage you to ask your doctor about the risk of post-surgical adhesion formation, and an estimate of need for future surgeries.
Related Content:
Avoid Surgeries: Adhesions | Blocked Fallopian Tubes | Endometriosis | PCOS | SBO | Surgery Risks | Tailbone