Discover lasting relief from post-hysterectomy pain with Clear Passage Physical Therapy’s Free Consult and Request Info – learn how their unique, non-surgical approach has helped countless women regain comfort and quality of life, and take the first step towards your personalized treatment plan today. To learn more visit our Apply to Therapy page.
We Treat Hysterectomy Pain Naturally, Without Surgery or Drugs
Hysterectomy is a major surgery performed in some of the deepest parts of the body. This surgery can cause adhesions to form, creating pain that lasts long after the surgery. Clear Passage® Physical Therapy is a world leader in the non-surgical, drug-free treatment of pelvic pain and adhesions, with over 30 years experience treating post-hysterectomy pain. Studies and citations published in peer-reviewed U.S. and international medical journals find that this physio/physical therapy decreased adhesion-related pelvic pain significantly.
Complete our online Request Consultation form to receive a free phone consultation with an expert therapist and learn whether our therapy can help you.
Hysterectomy Pain Overview
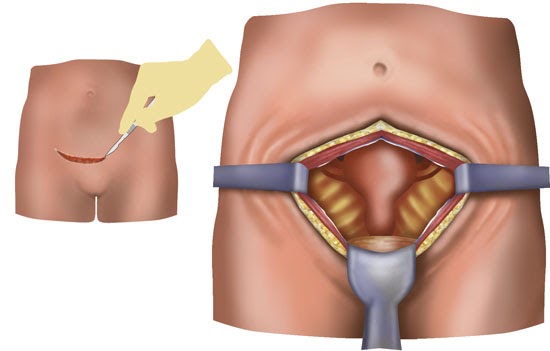
The most common surgical technique for hysterectomy is abdominal surgery. To access the uterus, the surgeon must first cut through several structures, including the skin and the peritoneum (tissue enclosing the abdominal and pelvic organs). After surgery, all of the cut tissues must heal.
Doctors generally expect complete recovery within four to eight weeks. For vaginal surgery, recovery usually occurs within one to two weeks. Either approach presents the possibility for adhesions to form deep within the abdomen, pelvis, or both.
Hysterectomy has become a fairly common surgery. In fact, so many women struggle with issues related to the pelvis that one in three women in the U.S. over age 60 has had a hysterectomy. (Office of Women’s Health, 2009b)
Of the 600,000 women who undergo hysterectomies in U.S. every year, most recover within the given time frame and return to pain-free lives. (Office of Women’s Health, 2009b) However, a study in 2007 found that 32% of women who underwent hysterectomies experienced chronic pelvic pain one year after their hysterectomy. The study also found that a vaginal surgery (rather than an abdominal surgery) did not significantly lower the risk of chronic pain. (Brandsborg et al., 2007)
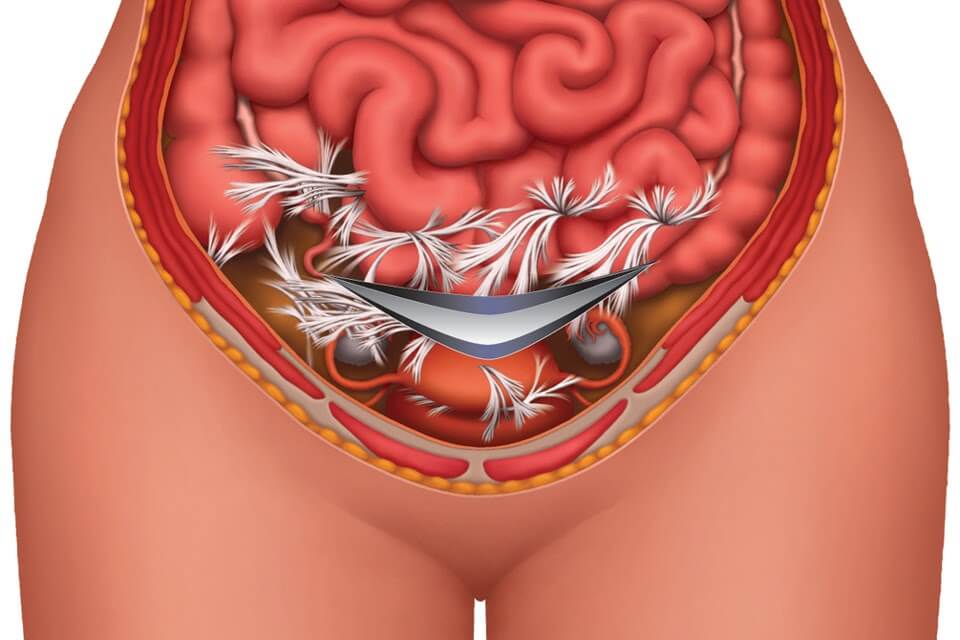
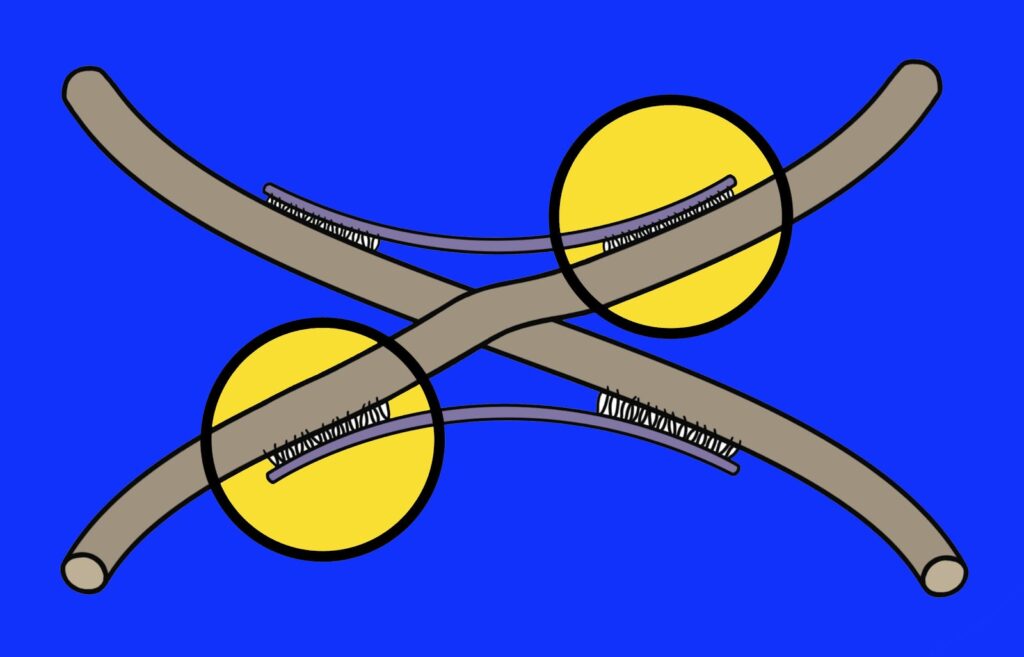
Adhesions are thick strands of collagen that form to help the body heal and repair after infection, trauma, surgery or various other injuries. Although the body needs these strands to help tissue repair, adhesions can spread, with the unwanted side-effect of binding and restricting structures that were previously mobile. This causes tightness in many women after a hysterectomy.
The tissues of the pelvis are extremely delicate and are meant to glide easily over each other. During a hysterectomy, the surgeon cuts or burns through pelvic tissues to remove the uterus and sometimes other structures. Tiny but powerful collagen fibers rush in to repair the tissues at the surgical sites. Attached to each other with molecular-chemical bonds called cross-links, the fibers create adhesions (internal scars) as the first step in the process of healing. Thus, adhesions form naturally after surgery. Pain and problems come when these adhesions spread. They can act like a powerful glue, binding neighboring structures – such as the intestines, bowels, vagina or bladder.
Symptoms of Adhesions After a Hysterectomy
When adhesions form after hysterectomy, women can experience a variety of side-effects, including:
- Pelvic or intercourse pain
- Low back pain (due to adhesive pulls into that area)
- Uncomfortable tightness or pulling
- Decreased desire, lubrication and orgasm
- Pain with or after urination
- Constipation or painful bowel movements
- Small bowel (intestinal) obstruction (SBO)
- Cramps after hysterectomy
- Tightness after hysterectomy
Symptoms can range from moderate discomfort to severe, recurring pain or tightness. In the case of SBO, they can become life-threatening as adhesions block the intestines, preventing food from passing thorough the digestive tract.
Intercourse pain and sexual dysfunction after hysterectomy
Following a hysterectomy, a woman can expect intercourse to be uncomfortable the first couple of times. If a woman has had one or both ovaries removed, she may also experience a decrease in lubrication and desire as her body goes through menopause.
If a woman feels pain with intercourse after six weeks, she may have a ‘mechanical’ problem such as vaginal adhesions or adhered pelvic ligaments. Many women feel that if they continue to try and push past the pain, the pain will eventually go away. If it doesn’t resolve after three or four attempts, we generally find that adhesions have formed in this area, pulling or restricting the vagina or attaching its delicate tissues to nearby structures, causing pain with intercourse.
The Journal of Sex & Marital Therapy classified female sexual function into six measurable domains: desire, arousal, lubrication, orgasm, satisfaction and pain. (Rosen et al., 2000) Although a woman who has undergone a hysterectomy may initially experience decreased function in these areas, function should return within a few weeks. If they do not, it is a sign that adhesions may be restricting the area, preventing normal sensation and function. In our published studies on this phenomenon, we found that treating the adhesions can significantly return function in these important areas.
Treatments
Clear Passage®️ Treatment
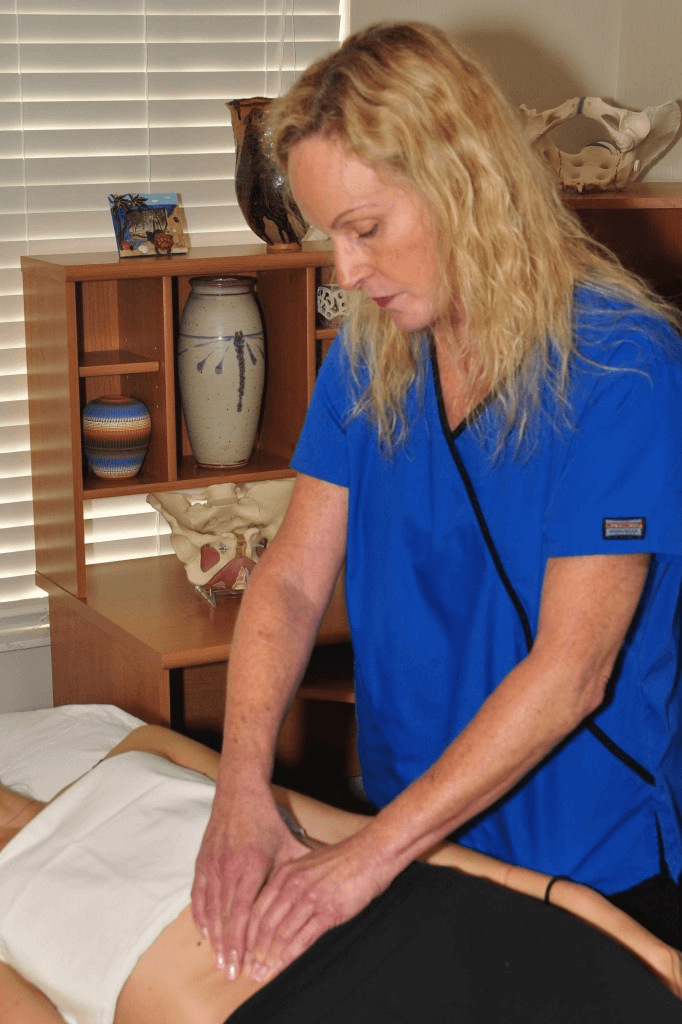
The Clear Passage® Approach is designed to reduce or eliminate adhesions cross-link by cross-link. It has been shown in numerous peer-reviewed medical journals to decrease pain and improve function without surgery or drugs.
We know pelvic adhesions well. Thirty years ago, our Director, physical therapist Belinda Wurn, developed severe adhesions after pelvic surgery and radiation therapy. Unable to work due to chronic pelvic pain and having seen the devastating and debilitating effects of pelvic adhesions in her own patients, she was determined to find a non-surgical way to address chronic pelvic pain and to decrease or eliminate pelvic adhesions.
With her husband, massage therapist Larry Wurn, Belinda took a much deeper look at the etiology and biomechanics of adhesion formation. They found that the molecular bonds that attached each of the tiny collagen fibers to its neighbor appeared to dissipate or dissolve with certain site-specific manual techniques. With this knowledge, they created the Clear Passage® approach to free adhesive bonds and return pain-sensitive structures to a more functional, pain-free state.
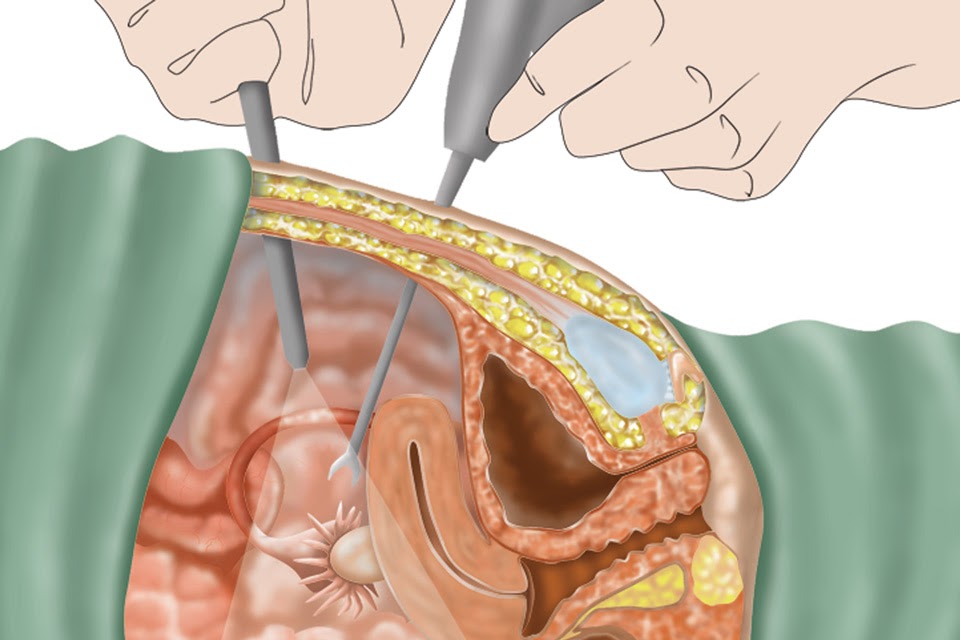
Other Treatments for Hysterectomy Pain (Surgery, Drugs)
Until recently, lysis (burning or cutting adhesions during laparoscopy or laparotomy) was the only option to remove adhesions in the pelvis. While lysis of pelvic adhesions can be effective, surgery has major drawbacks:
- It carries risks associated with anesthesia or infection.
- Surgeons can mistakenly cut of burn nearby or underlying structures.
- Despite the best skills of the finest surgeon, the body tends to create more adhesions as it heals from the very surgery designed to remove them.
A study in Digestive Surgery showed that 55% to 100% of women develop adhesions following pelvic surgery. Another study reported that 35 perfect of all open abdominal or pelvic surgery patients were readmitted to the hospital more than twice to treat post-surgical adhesions during the 10 years after their original surgery. Thus, pelvic surgery itself has been implicated as a major cause of adhesion formation and many patients become trapped in a cycle of surgery-adhesions-surgery – with no end in sight. Clear Passage®️ therapists provide the end to that cycle for many women.
Published Success Rates
To view a full list of our published success rates, please visit our Success Rates page.
Testimonials
To read past patient success stories, please visit our Testimonials page.