What are Pelvic Adhesions?
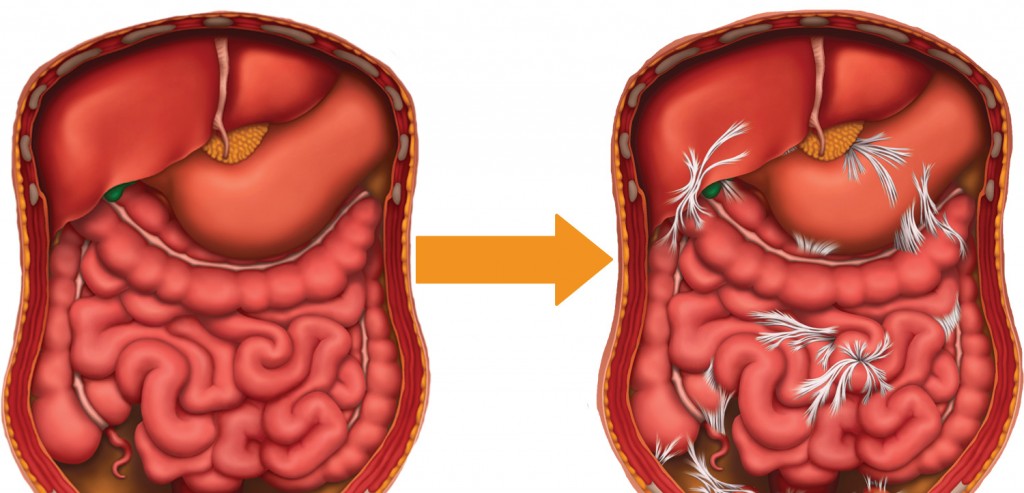
Many women are not receiving the education needed from their doctors about adhesions. Very few women even know they have adhesions. Most commonly known as “scar tissue,” adhesions are simply scar tissue that forms inside the body. Once formed, the body has no way to deal with the scar tissue so it will remain in place and sometimes spread to neighboring structures.
Adhesions consist of tiny strands of collagen that form around injured tissue as the body’s first step in the process of healing. Common areas of adhesion formation are areas affected by a prior infection, inflammation, or endometriosis. Pelvic adhesions can lead to a host of female health problems ranging from infertility to chronic pain including pain with intercourse. If you’ve had any kind of surgery, infection injury or endometriosis, there’s a good chance you have adhesions. We made a short guide that can help you figure out if you have adhesions after surgery.
What Causes Pelvic Adhesions?
- Surgery – Studies show that 55% to 100% of people who undergo pelvic surgery, will develop pelvic adhesions. Cutting into the delicate tissues near your reproductive structures can result in a large amount of scar tissue growing around the healing site. Many of the women we treat for secondary infertility or chronic pelvic pain have undergone a prior C-section, hysterectomy, or appendectomy (appendix removal.)
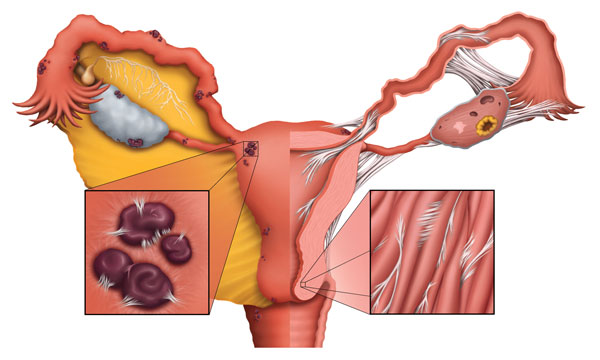
- Inflammation – Recurring inflammation is a very common cause of adhesions. Pelvic inflammatory disease (PID) is a major contributor to many of the infertility and pain cases we have treated. The constant inflammation causes scar tissue to grow in the pelvic area, often around the fallopian tubes or ovaries.
- Infection/STIs – Sexually Transmitted Diseases (STDs) can lead to chronic infection and inflammation which cause scar tissue to grow within the pelvis. The longer an infection or STD remains untreated, the more adhesions will form as the body attempts to surround and contain the infection. A major cause of blocked fallopian tubes is an untreated infection as a result of chlamydia or gonorrhea.
- Trauma – Contact sports, car accidents, falls or work-related injuries are common traumas that can cause the formation of pelvic adhesions. Since the body’s first step in healing is to create adhesions to contain and isolate the injury, almost everyone has adhesions somewhere in their body.
- Chronic conditions – Conditions that don’t have a definitive cure and recur periodically are considered chronic conditions. Two conditions responsible for a large portion of pelvic adhesions are polycystic ovarian syndrome (PCOS) and endometriosis. Both conditions share characteristics that result in adhesion formation. Chronic inflammation explained in detail above, and abnormal growths within a woman’s reproductive tract. PCOS gets its name from the cysts which form on a woman’s ovary. Both the cysts and the surgeries needed to remove the cysts will cause adhesions. Endometriosis is when endometrial tissue forms outside of the uterus. Endometriomas and endometrial implants can become inflamed and cause scar tissue to form around the site, causing endometriosis infertility, period, or intercourse pain.
- Radiation Therapy – We have treated many previous cancer patients for chronic pelvic pain because of radiation therapy. Radiation therapy is a treatment that can cause significant scarring and mechanical dysfunction inside a woman’s abdomen and pelvis. We often hear these patients describe their pain as a “stuck” or “tight” feeling that won’t go away.
Symptoms and Conditions Caused by Pelvic Adhesions
- Blocked fallopian tubes – One of the most common forms of infertility caused by adhesions is blocked fallopian tubes. Adhesions wrap around delicate structures inside the reproductive tract, preventing the reproductive system from working normally. Adhesions can restrict the flow of sperm through fallopian tubes, preventing the fertilization of an egg. Most physicians no longer perform surgery on these delicate structures, because post-surgical adhesions tend to block the tubes once again when the body heals from the surgery.
- Hydrosalpinx – Another common tubal blockage is a hydrosalpinx. This occurs when fluid collects in the fallopian tube – generally as the result of an infection. As adhesions form at the end of the tube closest to the ovary, the tube swells, much as your knee might swell after a knee injury. Hydrosalpinx usually indicates a totally blocked tube; in the rare case that the end is open, the sperm still tend to get lost in a large amount of fluid in the tube, greatly decreasing the chance for conception and increasing the chance for an ectopic pregnancy, in which the fertilized egg becomes stuck in the tube.
- Unexplained infertility – Adhesions don’t show up on most diagnostic tests. In order to verify that a patient has adhesions, an exploratory surgery is required to directly visualize the adhesions. Unfortunately, since most patients are unaware of adhesions, the question is never asked: “maybe my infertility is caused by adhesions?” This can lead to many women suffering from unexplained infertility.
- Prior surgery – Surgeries are sometimes necessary to save a woman’s life, as in the case of an appendectomy. There may be less urgency to perform surgery in the case of undiagnosed pain. In these cases, a doctor may suggest doing an exploratory surgery to directly visualize the pelvic contents. Because adhesions form after most pelvic surgeries, the very surgery to correct a problem can be the cause of adhesion formation as the body heals.
- Chronic pain – Stuck, tight, immobile, constantly uncomfortable. These are all common descriptions we hear from patients suffering from adhesions. Because adhesions bind to structures and create constant tension, it is no wonder why so many patients with adhesions also suffer from chronic pain.
- Sexual dysfunction – Some non-surgical treatments are available for women with intercourse pain (dyspareunia) or other sexual dysfunction. Studies on our work in this area have shown that women have an increase in every measurable criterion of their sexual health (desire, orgasm, lubrication, pain, and arousal) after being treated for adhesions.
Treatments for Pelvic Adhesions
Experience relief from debilitating pelvic adhesions with Clear Passage Physical Therapy’s Free Consult and Request Info – discover how their unique, non-surgical Clear Passage Approach has helped countless women overcome infertility, chronic pain, and sexual dysfunction caused by internal scarring, without the risks of additional surgery or medication. To learn more visit our Apply to Therapy page.
Few options exist for treating pelvic adhesions. Many treatments are aimed at treating the symptoms of adhesions, rather than the adhesions themselves. Following the Hippocratic Oath that all physicians should adhere to, we have always believed a natural, non-surgical, and drug-free approach should be the first step in the treatment of adhesions. Below are the options we see that have passed scientific scrutiny and been found to be effective, listed from safest to most invasive:
- Manual Physical Therapy – A non-surgical, all-natural treatment plan is what we consider the best treatment for adhesions. Clear Passage has been researching and treating patients with adhesions for over 25 years. The Clear Passage Approach (CPA) is a hands-on therapy that focuses on detaching and weakening adhesions inside the body. Helping patients have natural pregnancies, live a pain-free life, and avoid future surgeries is our number one goal.
If you or a woman you know is suffering from the symptoms above, we encourage you to complete a contact form or call us at 1-352-336-1433. You will be able to schedule a phone consultation with a member of our patient support team, at no cost, and learn whether our non-surgical and drug free treatment is right for you.
- Pain Medications – The rise in chronic pain conditions has been met with a rise in pain medication prescriptions. The opioid epidemic is a well-known phenomenon in America. Pain medication simply mask pain; they do nothing to address the cause of the pain. They do not provide permanent solutions; further, they can lead to severe digestive issues along with addiction and dependency. Pain medications should be considered a temporary palliative measure while the patient searches for an actual treatment.
- Surgery – Lysis (destruction) of adhesions by cutting or burning them during surgery is one of the most common ways to combat adhesion growth. Many surgeons note that this isn’t a permanent solution and often leads to more surgeries, because surgery is the number one cause of adhesions. Surgery also has risks, such as the risk of anesthesia, complications or infection and “inadvertent enterotomy” in which a surgeon mistakenly cuts into or through an organ s/he had not intended to, in the crowded and adhered structures of the pelvis.
Related Content:
- Adhesions and Scar Tissue
- Abdominal / Pelvic Adhesions
- Fascia and Fascial Adhesions
- What You Need to Know About Pelvic Adhesions
- Do Abdominal Adhesions Show on an MRI Scan?
- Patient Story: No Longer Shackled by Adhesions
- 3 Ways Adhesions Cause Bowel Obstructions
- How to Prevent Surgery Adhesions
- Adhesions in the Body: Presentation by Larry Wurn (Video)
- Break the Adhesion-Surgery Cycle
- Lifesaving Therapy for Intestinal Obstructions Comes to St. Louis
- Pelvic Adhesions: What You May Not Know
- What Are Adhesions? (Infographic)
- Adhesions: What You Can’t See Can Hurt You
- How Can Therapy Help Adhesions