BOWEL OBSTRUCTION SUCCESS RATES
Following the ‘scientific method’ for investigative new modalities, we began by publishing some remarkable case studies, all of which can be read on our Published Studies page. These studies included a woman who managed to stay alive despite a bowel that was virtually totally blocked. When she first arrived for therapy, it was clear that her only nutrition was through an intravenous PICC line. After several hours of therapy, her physician was able to remove her PICC line because she found she could eat normally. This and other surprising results inspired us to investigate further, with more involved studies.
Due to the complex structure and numerous functions of the bowel, measuring success in treating patients with recurring small bowel obstruction (SBO) presented several opportunities. In short, we found three major areas of concern that we could measure by comparing conditions before and after therapy:
- Structure – Independent radiographic images taken before and after therapy
- Repeat Events – Number of repeat obstructions before and after therapy
- Quality of Life – Graded by patient, results tabulated by biostatisticians
STRUCTURE – BEFORE AND AFTER X-RAYS
Some patients allowed us to document the structure of their intestines by undergoing a “small bowel follow-through” test (SBFT) before and after therapy. In this test, the patient would swallow a cocktail that contained a barium tracer, which would give precise images of the interior of the bowel. Concerned that they might obstruct the test, many patients avoided taking this test, which involves swallowing a rather thick liquid with a radio-opaque barium tracer. Nevertheless, the test does give a good picture of the inside of the bowel; it can show where narrowing or obstructions might be occurring. Using this test, we’ve been able to get some very clear images that document bowel obstructions in patients who arrive for therapy, and the result of our hands-on care on their previously blocked intestines.
In the images shown here, one can clearly see the progress of the liquid (shown in white) as it passes through the small intestine, and where it becomes blocked. These images give dramatic testament to the positive changes we can actually see, in ‘before and after’ images.
In the two-part image shown here, we see in the image taken “Before” therapy, an hourglass-shaped stricture (narrowing) is visible in this patient’s intestines. The constriction is so significant that very little dye goes through to the bowels below, beyond the stricture. In fact, the patient was scheduled for emergency surgery before we treated her. Instead, she decided to try Clear Passage® therapy first.
Comparing that with the “After” image, one can easily see that the stricture completely resolved (disappeared) after therapy designed to clear adhesions from the area. Notice also how open the intestines are above and below the site of the prior stricture, in the areas beyond the previously narrowed bowel. The radiologist cited this as a “normal bowel” after therapy.
In the second set of images, we see a very dramatic string stricture “Before” therapy. This is a 3-inch-long section where the contents of the bowel are passing through an area that is narrowed to the size of a coffee straw. Certainly, no food was going to pass through this area. Again, this patient opted to first try Clear Passage® therapy, rather than undergo abdominal surgery to repair her bowel.
In the image taken “After” therapy, we can see that the area that was once so narrow for its entire length has broadened dramatically. In fact, this radiologist noted after therapy, “This patient now has a normal bowel.”
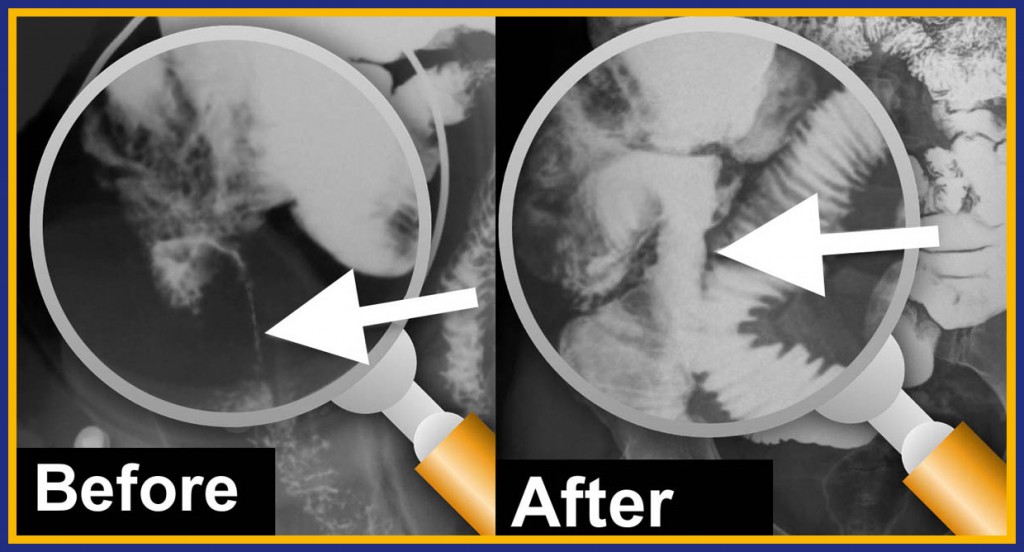
We have published other similar “before and after” images, but these are clearly quite clear and demonstrative. Once thought impossible, these images clearly demonstrate the effectiveness of a manual therapy, designed and tested for its ability to decrease adhesions, to dramatically improve the structure of the bowel.
REPEAT EVENTS – DECREASING RECURRING OBSTRUCTIONS
Surgery as a Cause of SBO
It is a well-known fact that surgery is the primary cause of bowel obstruction. No matter how compassionate, brilliant, or skilled the surgeon, the body must heal from the cuts or burns imposed by the surgery. The first step in the process of healing from surgery is the laying down of adhesions (scar tissue) in a random pattern over the tissue that has been damaged. Thus, the surgery designed to cure the obstruction can be the cause of the next obstruction.
Unwanted Complications
In some cases, a drop of bacteria-laden bowel contents can leak unseen into the abdomen before the physician closes the patient. Set free in this warm, moist, and dark environment, bacteria can proliferate quickly. Perhaps for that reason, roughly one in five (18 % per HHS) of all bowel resection patients are readmitted to the hospital within 30 days of their SBO surgery, often for peritonitis or other infection that occurs when bacteria freed from the intestine grow in the post-surgical abdomen. In this case, the physician will often reopen the patient surgically to introduce antibiotics directly into the infected spaces. The surgeon may choose to leave the body open to continue to administer medications directly into the abdomen and allow scarring to occur from the inside out to treat all of the infection. Naturally, this tends to create even more adhesions.
Even for those who are not re-admitted to the hospital during the month after surgery, the chance of a repeat obstruction caused by a prior surgery is too high. While surgery is routinely cited as the primary cause of bowel obstruction, a recent study in the Journal of the American Medical Association[i] notes that bowel resection is the 2nd most common emergency surgery in the U.S.A. and carries the highest complication rate (47%). The mortality rate was 6.5%, so 1 in 15 died during or after the procedure.
Most of our SBO patients are too familiar with the problem of repeat obstructions. They come to us with the goal of “no more obstructions.” They tell us they are tired of a lifetime of wondering, “Is this the day I’m going to die?” or “Is this the day I’m going to have to be struck down with severe pain and have to go to an emergency room with an obstruction?” Our patients ask us about their chances of avoiding future obstructions so they can get back to living their lives without dread or uncertainty. In order to give a truthful answer, we put this question to our research staff.
To conduct a study of this nature, we enlisted the help of physicians and researchers from several medical schools, including Harvard, Stanford, Washington University, the University of Florida, and of Arizona. Their guidance helped design a controlled study of 239 patients who were experiencing recurring bowel obstructions.
We treated 103 of the patients (the Therapy Group) and did not treat 136 of them (the Control Group). The typical Therapy patient received our usual protocol: 20 hours of Clear Passage® treatment over 5 days. Control patients received the present Standard of Care, which is no therapy. We measured repeat Total and Partial Obstructions and Repeat Surgeries 90 days after the study closed.
Results (shown here) were remarkable. The group we did not treat had 15 times more total bowel obstructions than those we treated. In fact, less than 1% of the patients we treated underwent another total bowel obstruction measured 90 days after the study closed. By contrast, close to 15% of the Controls (no therapy) had another total obstruction within the same 90-day period. Measured in both statistical and humanitarian ways, we found these results to be wonderful.
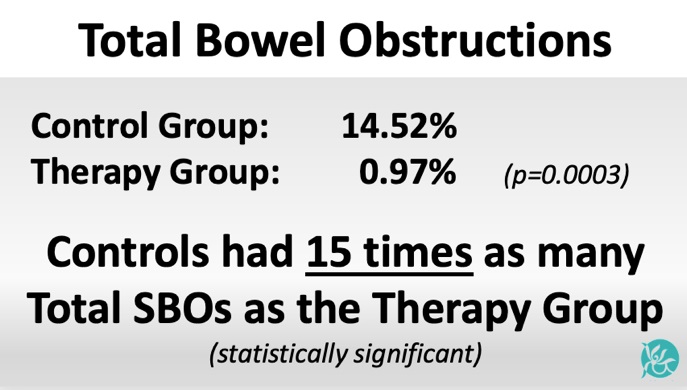
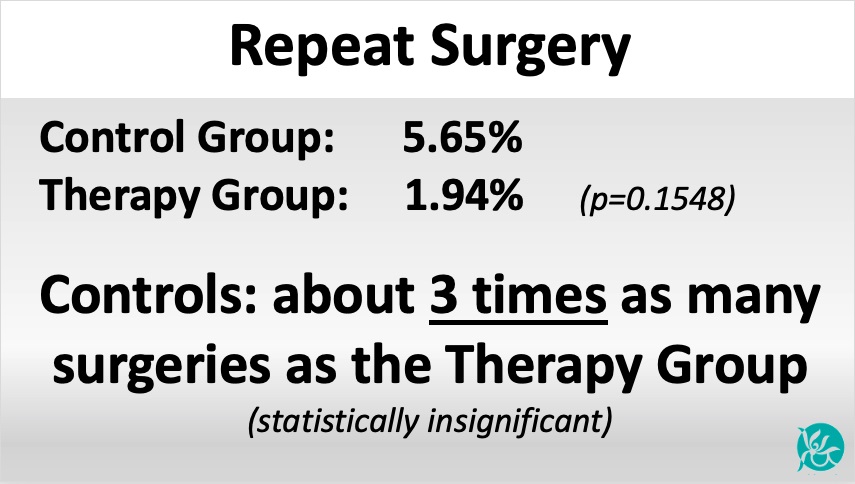
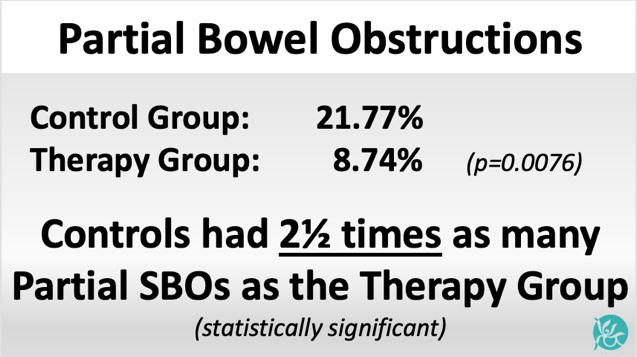
As shown in these images, the untreated group also had 2½ times more partial obstructions and 3 times as many surgeries as the patients we treated.
IMPROVING QUALITY OF LIFE
We find quality of life to be an important measure of success for patients who have undergone the traumas of bowel obstruction (with or without surgery), followed by years of fear of having another one or more. So many of these patients are miserable, often in pain, frustrated at a medical system they feel has let them down. Many report that their physicians say, “there’s nothing you can do to change this.” We are glad that our therapy is beginning to turn that attitude around.
Virtually all of these people live in fear of another obstruction that could happen at any time. Thus, we hired a biostatistician to design, validate, and publish a questionnaire and rating tool to measure quality of life in the five major ‘domains’ where they report problems:
- Diet
- Pain
- Medication
- Quality of Life Issues, and
- Gastrointestinal (GI) Symptoms
Read more about bowel obstruction self-care.
The questionnaire was given to patients when they enrolled in the study, and then again 90 days after the study closed. The biostatistician was able to measure changes (if any) between the start and end dates for both the Therapy and the Control Group.
Realizing that both the degree of pain and the ability to move freely affect Quality of Life, we added a “pain rating” section and a section that compared ‘before and after’ Trunk Range of Motion for each participant.
- The Diet Domain assessed the diet of the subject from inability to tolerate any liquid to a normal solid food diet.
- The Pain Domain reported pain throughout the body, with oral intake of food or liquid, and with bowel function.
- The Gastrointestinal (GI) Symptom Domain quantified symptoms often associated with SBO, such as nausea, emesis, bowel spasm, and constipation.
- The Medication Domain reports the frequency of medications required to maintain bowel function.
- The Quality of Life Domain quantified the amount of time off work and social activities. In addition, it quantified each patient’s overall concern regarding their bowel function. We found that all of these tend to be major lifetime concerns for many people who experience recurring bowel obstructions.
QUALITY OF LIFE – STATISTICALLY MEASURED RESULTS
A Note on Statistics
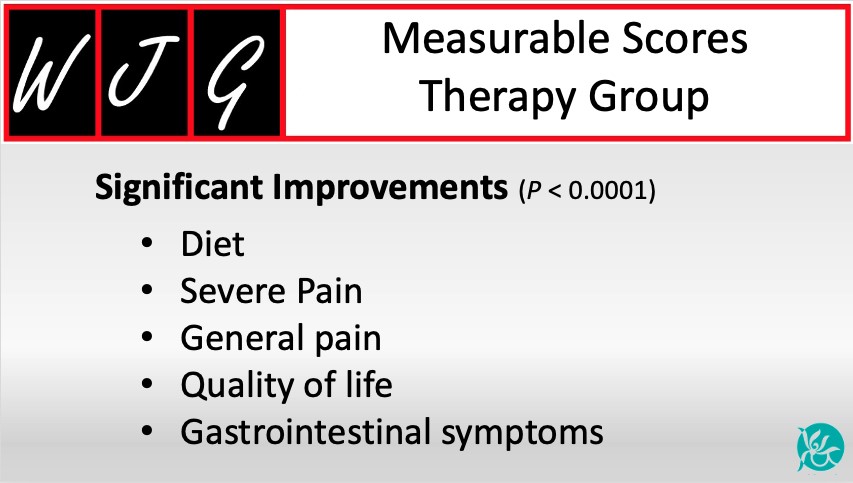
Statisticians measure results by asking, “What is the chance this result could have occurred by chance?” In this study, they used the common statistical measure (p=.05). This means if the measure is smaller than “5 out of 100”, the result is statistically significant (reliable). Any number greater than “.05” is considered clinically insignificant (unreliable). The data in the controlled study shown here, and published in the prestigious World Journal of Gastroenterology, showed very high statistical significance (reliability) at p<0.0001. Thus, the chance that the numbers are unreliable was less than 1 out of 10,000 for Clear Passage® patients in the domains shown below. In essence, these results are considered highly reliable.
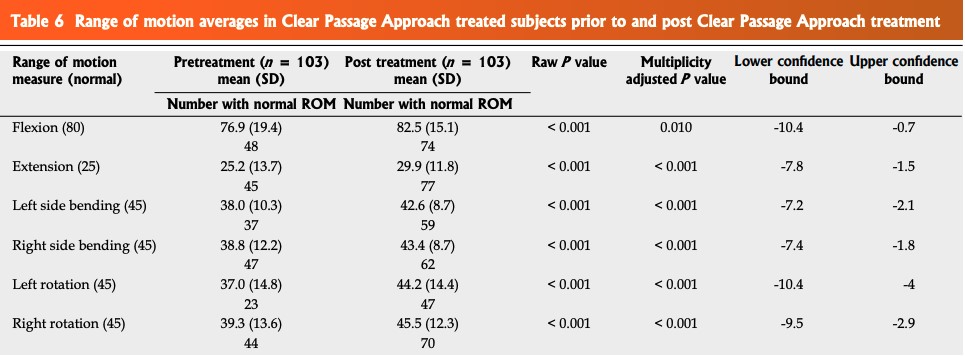
Trunk Range of Motion measurements showed that all Clear Passage® patients demonstrated overall improvement in Range of Motion (p<0.0001) extrapolated statistically in the table below.
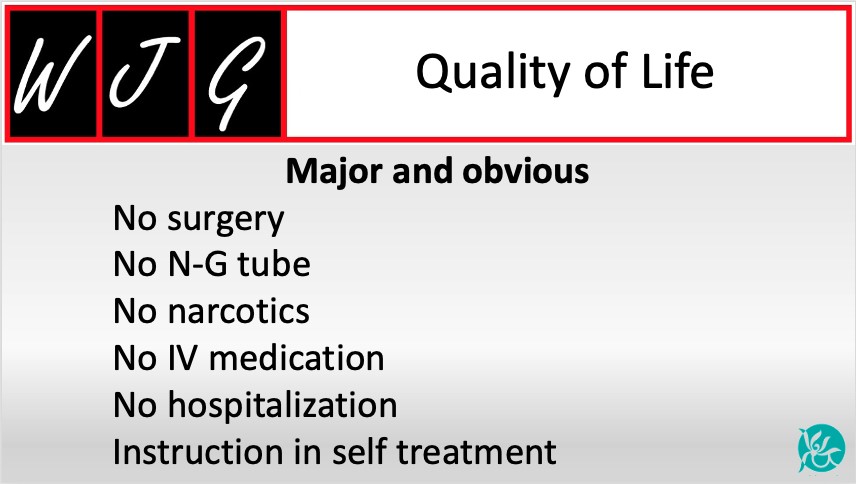
In addition to the statistical measures shown above, the journal notes or implies other major or obvious Quality of Life advantages of Clear Passage over the present Standard of Care (no therapy). These tend to include hospitalization, insertion of an NG tube, intravenous hydration, possible surgery, and ongoing fear of another obstruction. (The difference in this fear was significant in the Quality of Life domain.) These “other advantages” are shown here in an image labeled Quality of Life.
RESULTS (direct quote from the study)
Despite histories of more prior hospitalizations, obstructions, surgeries, and years impacted by bowel issues, the 103 CP-treated subjects reported a significantly lower rate of repeat SBO than 136 untreated controls (total obstructions P = 0.0003; partial obstructions P = 0.0076).
Subjects treated with the therapy demonstrated significant improvements in five of six total domains in the validated Small Bowel Obstruction Questionnaire (SBO-Q).
Domains of diet, pain, gastrointestinal symptoms, quality of life (QOL), and pain severity when compared to post CPA treatment were significantly improved (P < 0.0001).
The medication domain was not changed in the CPA treated group (P = 0.176).
A Note on Comparing Groups
In all controlled studies, researchers try their best to gather identical groups. This process can be challenging and costly. While large medical schools generally have the funding to do this, our small group lacked that option. This was a major disadvantage for us.
As our study developed, we realized that patients in the group we treated (the CP Therapy Group) averaged 18 years older than untreated subjects. In addition, those in the CP Therapy Group had roughly double the number of prior surgeries, partial bowel obstructions, and years impacted with bowel symptoms than people in the Control Group.
The biostatistician noted statistical significance that the CP-treated patients:
- Averaged 18 years older 54.5 vs 36.4
- Averaged over twice as many prior surgeries 4.56 vs 2.07
- Averaged over twice as many partial obstructions 3.97 vs 1.88
- Averaged being impacted by SBOs for twice the number of years 10.7 vs 5.5
The Controls did report a few more prior total SBOs, but the numbers were considered so close that the biostatistician judged that statistically insignificant 1.68 vs 2.17
Because patients in the Therapy Group had much more complex histories, the authors expected that group to do much worse than the Controls. Given the above, it is perhaps even more remarkable that after the study concluded, untreated patients had:
15 times more total obstructions,
2.5 times more partial obstructions, and
3 times as many surgeries as the ones treated by Clear Passage®.
[i] Scott JW, Olufajo OA, Brat GA, et al. Use of National Burden to Define Operative Emergency General Surgery. JAMA Surg. 2016;151(6):e160480. doi:10.1001/jamasurg.2016.0480
Related Content:
Research and Success Rates
- Study Results for a Non-Surgical Bowel Obstruction Treatment
- Study Results for a Non-Surgical Bowel Obstruction Treatment
- Bowel Obstruction Success Rates
Questions Answered
- Recurring Small Bowel Obstruction Treatment Frequently Asked Questions
- The Most Common Causes of Bowel Obstruction and How to Prevent It
- Bowel Blockage Symptoms
- How to Prevent Bowel Obstruction
- Can Diverticulitis Cause Bowel Obstruction?
- Seven Signs of Intestinal Blockage
- What to know before accepting an IBS Diagnosis
- How Long Does a Bowel Obstruction Last?
- What is the Cause of a Small Bowel Obstruction and What Are Your Options for Treatment?
- How Will My Lifestyle Change with Small Bowel Obstructions?
- Is There a Natural Treatment for Small Bowel Obstruction?
- What SBO Patients Can Expect From Treatment
Treatment
- At a Glance: Bowel Obstruction
- Bowel Obstruction
- Bowel Obstruction – Need Help Now?
- Bowel Obstruction Treatment
- [Infographic] The Main Causes of Bowel Obstructions
Patient’s Stories
- Bowel Obstruction: Patient Story Update
- Video Testimonial – A Mother’s Journey to Recovery: Small Bowel Obstruction
- What Is Bowel Obstruction? – A Patient’s Perspective
- A Glimpse into a Brave Young Boy’s Journey with CHARGE Syndrome
- Success Story: Clear Passage Allowed Me to Resume My Adventures
- Emergency Small Bowel Obstruction Surgery in India
- An End to Bowel Obstructions
Diet
- How to Relieve a Bowel Obstruction: Diet Guide
- Recipes For Bowel Obstruction Patients
- Diet Guide for Avoiding Bowel Obstruction
- Diet Modifications to Help You Handle a Small Bowel Obstruction
- Digestive Health Guide
- Bowel Obstruction: Diet & Lifestyle Recommendations
- Minimal Fiber Diet for Digestive Disorders
- Nutritional Guidelines
- Transitioning to a Regular Diet from a Low or Minimal Fiber Diet
- Low Fiber Diet for Digestive Disorders
Bowel Obstruction | SBO | SIBO